1. Marjan AQ, Marliyati SA. Relationship between food consumption and physical activity with risk of osteoporosis in elderly at nursing home in bogor. J Gizi Pangan 2013;8:123-8.
https://doi.org/10.25182/jgp.2013.8.2.123-128.

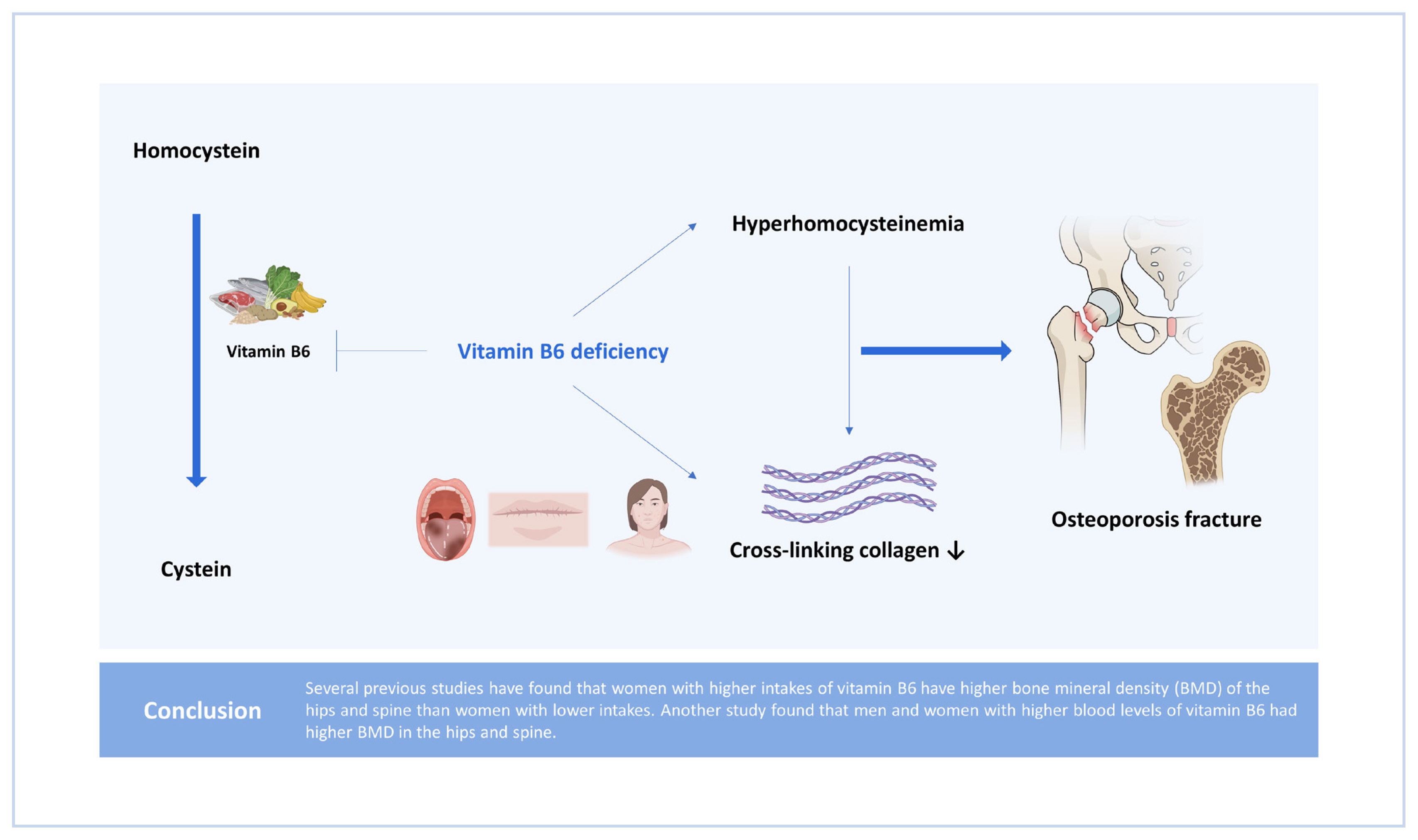
2. Farapti , Sayogo S. The benefits of vitamin B6 in osteoporotic fractures. Cermin Dunia Kedokteran 2013;40:751-5.
3. Umamah F, Rahman F. Umamah, rahman: Hubungan senam osteoporosis dengan kejadian osteoporosispada peserta senam di rumah sakit islam surabaya. J Ilm Kesehatan 2016;9:114-20.
https://doi.org/10.33086/jhs.v9i2.157.

5. Limbong EA, Syahrul F. Risk ratio of osteoporosis according to body mass index, parity, and caffein consumption. J Berkala Epidemiol 2015;3:194-204.


7. Dwi Alifatul H, Santi M. The relationship between obesity and osteoporosis (Study at Husada Utama Hospital Surabaya). J Berkala Epidemiol 2013;1:172-81.
8. Ruan J, Gong X, Kong J, et al. Effect of B vitamin (folate, B6, and B12) supplementation on osteoporotic fracture and bone turnover markers: a meta-analysis. Med Sci Monit 2015;21:875-81.
https://doi.org/10.12659/msm.893310.



9. Almatsier S. Prinsip dasar ilmu gizi. Jakarta, ID: Gramedia; 2001.
11. Setiawan B, Rahayuningsih S. Angka kecukupan vitamin larut air. Widayakarya Nasional Pangan dan Gizi. In: Paper presented at: Prosiding Angka Kecukupan Gizi dan Acuan Label Gizi. 2004 May 17-19; Jakarta, ID: Widayakarya Nasional Pangan dan Gizi; pp 75-99.
12. Herrmann M, Peter Schmidt J, Umanskaya N, et al. The role of hyperhomocysteinemia as well as folate, vitamin B(6) and B(12) deficiencies in osteoporosis: a systematic review. Clin Chem Lab Med 2007;45:1621-32.
https://doi.org/10.1515/cclm.2007.362.


14. Gröber U. Mikronutrien: Penyelarasan metabolik, pencegahan, dan terapi. Pengarang, ID: Penerbit Buku Kedokteran; 2012.
17. Koh JM, Lee YS, Kim YS, et al. Homocysteine enhances bone resorption by stimulation of osteoclast formation and activity through increased intracellular ROS generation. J Bone Miner Res 2006;21:1003-11.
https://doi.org/10.1359/jbmr.060406.


18. van Wijngaarden JP, Doets EL, Szczecińska A, et al. Vitamin B12, folate, homocysteine, and bone health in adults and elderly people: a systematic review with meta-analyses. J Nutr Metab 2013;2013:486186.
https://doi.org/10.1155/2013/486186.



20. Yazdanpanah N, Zillikens MC, Rivadeneira F, et al. Effect of dietary B vitamins on BMD and risk of fracture in elderly men and women: the Rotterdam study. Bone 2007;41:987-94.
https://doi.org/10.1016/j.bone.2007.08.021.


21. McLean RR, Jacques PF, Selhub J, et al. Plasma B vitamins, homocysteine, and their relation with bone loss and hip fracture in elderly men and women. J Clin Endocrinol Metab 2008;93:2206-12.
https://doi.org/10.1210/jc.2007-2710.



22. Green TJ, McMahon JA, Skeaff CM, et al. Lowering homocysteine with B vitamins has no effect on biomarkers of bone turnover in older persons: a 2-y randomized controlled trial. Am J Clin Nutr 2007;85:460-4.
https://doi.org/10.1093/ajcn/85.2.460.


23. Holstein JH, Herrmann M, Splett C, et al. Low serum folate and vitamin B-6 are associated with an altered cancellous bone structure in humans. Am J Clin Nutr 2009;90:1440-5.
https://doi.org/10.3945/ajcn.2009.28116.


24. Saito M, Marumo K. Collagen cross-links as a determinant of bone quality. In: Shimada Y, Miyakoshi N, editors. Osteoporosis in orthopedics. Tokyo, JP: Springer; 2016. p.35. -54.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






