3. Dash SK, Panigrahi R, Palo N, et al. Fragility hip fractures in elderly patients in Bhubaneswar, India (2012-2014): A prospective multicenter study of 1031 elderly patients. Geriatr Orthop Surg Rehabil 2015;6:11-5.
https://doi.org/10.1177/2151458514555570.



6. Neuburger J, Currie C, Wakeman R, et al. The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England: an external evaluation using time trends in non-audit data. Med Care 2015;53:686-91.
https://doi.org/10.1097/mlr.0000000000000383.



7. Cha YH, Lee YK, Koo KH, et al. Difference in mortality rate by type of anticoagulant in elderly patients with cardiovascular disease after hip fractures. Clin Orthop Surg 2019;11:15-20.
https://doi.org/10.4055/cios.2019.11.1.15.



8. Cha YH, Ha YC, Park HJ, et al. Relationship of chronic obstructive pulmonary disease severity with early and late mortality in elderly patients with hip fracture. Injury 2019;50:1529-33.
https://doi.org/10.1016/j.injury.2019.05.021.


9. Cha YH, Ha YC, Yoo JI, et al. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg 2017;137:625-30.
https://doi.org/10.1007/s00402-017-2674-2.


11. Finsterwald M, Sidelnikov E, Orav EJ, et al. Gender-specific hip fracture risk in community-dwelling and institutionalized seniors age 65 years and older. Osteoporos Int 2014;25:167-76.
https://doi.org/10.1007/s00198-013-2513-4.


14. Kristensen PK, Johnsen SP, Mor A, et al. Is the higher mortality among men with hip fracture explained by sex-related differences in quality of in-hospital care? A population-based cohort study. Age Ageing 2017;46:193-9.
https://doi.org/10.1093/ageing/afw225.


16. Marques EA, Carballido-Gamio J, Gudnason V, et al. Sex differences in the spatial distribution of bone in relation to incident hip fracture: Findings from the AGES-Reykjavik study. Bone 2018;114:72-80.
https://doi.org/10.1016/j.bone.2018.05.016.



17. Min J. Re: “Age and sex differences in body mass index as a predictor of hip fracture: A NOREPOS Study”. Am J Epidemiol 2017;185:511.
https://doi.org/10.1093/aje/kwx026.


19. Power J, Loveridge N, Kröger H, et al. Femoral neck cortical bone in female and male hip fracture cases: Differential contrasts in cortical width and sub-periosteal porosity in 112 cases and controls. Bone 2018;114:81-9.
https://doi.org/10.1016/j.bone.2018.05.027.


21. Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009;301:513-21.
https://doi.org/10.1001/jama.2009.50.


22. Wang CB, Lin CF, Liang WM, et al. Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone 2013;56:147-53.
https://doi.org/10.1016/j.bone.2013.05.015.


23. Cheol Seong S, Kim YY, Khang YH, et al. Data resource profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol 2017;46:799-800.
https://doi.org/10.1093/ije/dyw253.



25. Lee J, Lee JS, Park SH, et al. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol 2017;46:e15.
https://doi.org/10.1093/ije/dyv319.


26. Seong SC, Kim YY, Park SK, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 2017;7:e016640.
https://doi.org/10.1136/bmjopen-2017-016640.



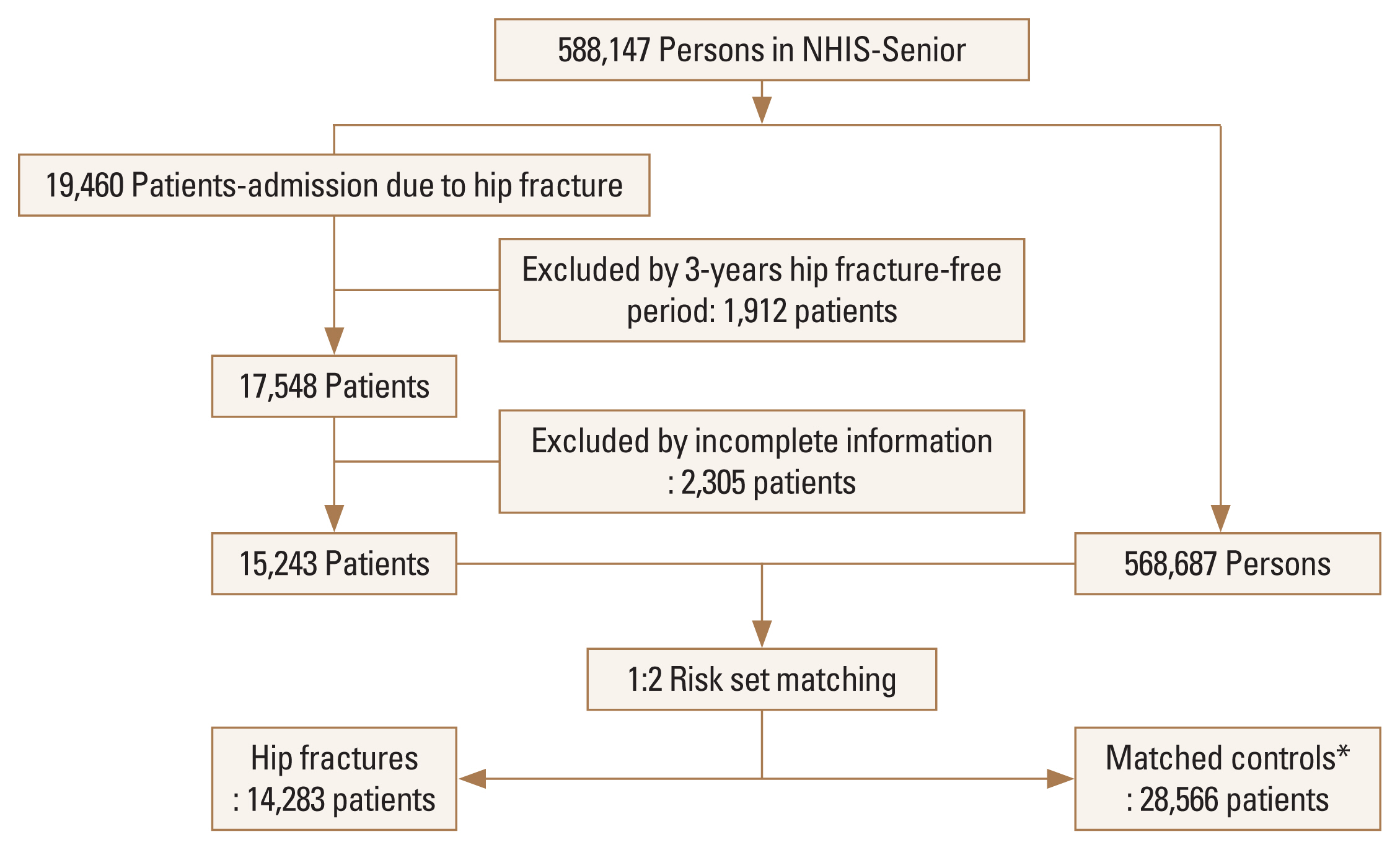
27. Park C, Jang S, Jang S, et al. Identification and validation of osteoporotic hip fracture using the National Health Insurance Database. J Korean Hip Soc 2010;22:305-11.

30. Jang SY, Cha YH, Kim KJ, et al. The effect of surgery type on mortality in elderly patients with pertrochanteric femoral fracture: A Korean nationwide cohort study. Asian J Surg 2020;43:550-6.
https://doi.org/10.1016/j.asjsur.2019.06.006.


31. Li YP, Propert KJ, Rosenbaum PR. Balanced risk set matching. Journal of the American Statistical Association 2001;96:870-82.

34. Andersen LW, Granfeldt A, Callaway CW, et al. Association between tracheal intubation during adult in-hospital cardiac arrest and survival. JAMA 2017;317:494-506.
https://doi.org/10.1001/jama.2016.20165.



35. Suissa S, Moodie EE, Dell’Aniello S. Prevalent new-user cohort designs for comparative drug effect studies by time-conditional propensity scores. Pharmacoepidemiol Drug Saf 2017;26:459-68.
https://doi.org/10.1002/pds.4107.


36. Yoo KD, Kim CT, Kim MH, et al. Superior outcomes of kidney transplantation compared with dialysis: An optimal matched analysis of a national population-based cohort study between 2005 and 2008 in Korea. Medicine (Baltimore) 2016;95:e4352.
https://doi.org/10.1097/md.0000000000004352.



37. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 2014;33:1242-58.
https://doi.org/10.1002/sim.5984.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






