 |
 |
| jbm > Volume 31(1); 2024 > Article |
|
Abstract
Sarcopenia, which is characterized by an age-related decline in muscle mass and function, poses significant challenges to geriatric care. Its definition has evolved from muscle-specific criteria to include muscle mass, muscle function, and physical performance, recognizing sarcopenia as a physical frailty. Sarcopenia is associated with adverse outcomes, including mortality, falls, fractures, cognitive decline, and admission to long-term care facilities. Neuromechanical factors, protein-energy balance, and muscle protein synthesis-breakdown mechanisms contribute to its pathophysiology. The identification of sarcopenia involves screening tests and a comprehensive assessment of muscle mass, strength, and physical function. Clinical approaches aligned with the principles of comprehensive geriatric assessment prioritize patient-centered care. This assessment aids in identifying issues related to activities of daily living, cognition, mood, nutrition, and social support, alongside other aspects. The general approach to factors underlying muscle loss and functional decline in patients with sarcopenia includes managing chronic diseases and evaluating administered medications, with interventions including exercise and nutrition, as well as evolving pharmacological options. Ongoing research targeting pathways, such as myostatin-activin and exercise mimetics, holds promise for pharmacological interventions. In summary, sarcopenia requires a multifaceted approach, acknowledging its complex etiology and tailoring interventions to individual patient needs.
Sarcopenia is a condition characterized by a decrease in muscle mass and a decline in muscle function (muscle strength or physical function), which occurs with aging.[1] Sarcopenia was initially defined based on the distribution of muscle mass in the young adult population, with criteria such as having muscle mass below a certain level (e.g., more than 2 standard deviations below the average) indicating sarcopenia.[2,3] However, studies emphasized the clinical importance of both muscle mass and muscle function in various population groups, particularly in the 2010 European Working Group on Sarcopenia in Older People (EWGSOP) guidelines, which began to define sarcopenia based on both criteria.[4] Subsequently, numerous epidemiological and intervention studies in various populations and settings have been conducted, leading to the development of various definitions, including the Foundation for the National Institutes of Health (NIH) criteria of the U.S. NIH,[5] the revised EWGSOP2,[6] and the updated Asian Working Group on Sarcopenia (AWGS) 2019 criteria,[7] which built upon the 2014 AWGS criteria.[8] Interestingly, the Sarcopenia Definitions and Outcomes Consortium and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis, and Musculoskeletal Diseases (ESCEO) stated that muscle function is more important than muscle mass, in diagnosing sarcopenia and assessing clinical improvement.[9] In 2023, the Korean Working Group on Sarcopenia (KWGS) published clinical practice guidelines for screening and diagnosing sarcopenia in older Korean adults.[10,11]
Since the prevalence of sarcopenia in the population increases with age, and its pathophysiology is associated with various age-related mechanisms or outcomes, it is regarded as both an aging-related condition and a geriatric syndrome.[12] Additionally, sarcopenia can be considered as a mobility phenotype of the human aging spectrum owing to its focus on muscle mass and function. Frailty is a spectrum of clinical phenotype that reflects a person’s biological age, and physical frailty and sarcopenia share several phenotypic and clinical aspects, leading to the operational definition of a common syndrome referred to as “physical frailty and sarcopenia”.[13,14] The clinical outcomes of sarcopenia ultimately lead to adverse outcomes, including falls, mortality, and admission to long-term care facilities due to functional decline, for many older adults.[12,15-17] As a result, the importance of sarcopenia in the field of geriatrics has increased, in line with the global aging population. In 2016, the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) officially classified sarcopenia as a disease,[18] and in South Korea, sarcopenia was classified as M62.5 in the 8th edition of the Korean Standard Disease Classification (KCD-8) in 2021.
Interpreting the prevalence of sarcopenia in the population requires careful consideration, given the absence of a worldwide consensus on its definition.[19] Additionally, the cut-off points for evaluating the components of sarcopenia such as muscle mass, muscle strength, and physical function are typically determined based on the distribution of these factors in the population. Notably, when applying the distribution of healthy young adults to older adults, the calculated prevalence of sarcopenia in literature is subject to the influence of changes in birth cohort characteristics due to socio-economic changes.
Consequently, the prevalence of sarcopenia varies significantly depending on the characteristics of the population (e.g., age structure, urban, or rural), definition of sarcopenia, and types of items assessed. Based on domestic study, the prevalence of sarcopenia in the older population in South Korea ranges from 4% to 45%.[20] According to the Korean Frailty and Aging Cohort Study (KFACS), when applying the AWGS 2019 criteria to the population aged 70 years and older, 26.8% of men and 18.8% of women met the criteria for low muscle mass and function (e.g., handgrip strength, gait speed, or the ability to rise from a chair).[21] Other local community studies in South Korea have reported the prevalence of sarcopenia.[22,23]
When conducting longitudinal observations in community-dwelling older individuals, sarcopenia has been reported to be associated with various adverse outcomes, including overall mortality, falls, fractures, physical and cognitive function decline, impairment of activities of daily living, reduced quality of life, and admission to care facilities due to functional decline.[12,24-26] Furthermore, in studies involving patients admitted to hospitals for various individual diseases, sarcopenia has been found to predict complications during inpatient or surgical treatments.[27] This association has been actively reported in clinical scenarios such as cardiac surgery, liver transplantation, kidney transplantation, various solid tumor surgeries, and adjuvant/palliative chemotherapy for cancer.[27,28]
As a geriatric syndrome, the phenotype of sarcopenia is influenced by various biological mechanisms associated with aging and physiological and biochemical changes resulting from multiple diseases that accumulate with age. The pathogenesis of sarcopenia involves not only biological changes but also functional (e.g., decreased instrumental activities of daily living, and difficulties in swallowing and in performing tasks) and social and economic (e.g., economic poverty, widowhood, or living alone) factors.[29] Furthermore, similar to the concept of frailty, sarcopenia and its resulting functional decline create a vicious cycle, accelerating muscle mass loss and loss of physical function.[12,14] The impact of these mechanisms varies among individuals and can be broadly classified into three main mechanistic groups: (1) neuro-mechanical factors; (2) protein-energy balance; and (3) muscle protein synthesis-breakdown mechanism. These three groups are not mutually exclusive and can interact with one another, impacting muscle protein synthesis and function. Ultimately, they play a crucial role in determining the long-term loss of muscle mass.
Neuro-mechyanical factors are considered the most critical in the prevention and intervention of sarcopenia when viewed individually.[30] They encompass various aspects such as physical activity, resistance exercise, the efficiency of exercise neurons, and neuromuscular junctions, as well as mechanical transitions.[31] The costamere, a collection of proteins that connect the extracellular matrix to the sarcomere, transmits mechanical stimuli to mechanistic target of rapamycin complex 1 (mTORC1) through phosphorylation mechanisms called mechanotransduction.[32,33] Studies in humans have shown that muscle protein synthesis increases in the hours to 72 hr after a single bout of resistance exercise.[34,35] These short-term changes and long-term resistance training can improve efficiency of mitochondria and muscle protein synthesis-breakdown mechanisms, playing a vital role in maintaining muscle mass and muscle function.[36,37] In addition to increasing muscle mass, physical activity, including resistance exercise, can independently enhance muscle function.[30] For example, remodeling of neuromuscular junctions can improve motor unit recruitment even in the absence of increased muscle mass, leading to improved muscle function.[38] Conversely, muscle strength decreases daily by 1% with continued bed rest.[39]
Protein and energy intake, including micronutrient intake, significantly impact muscle protein synthesis and breakdown.[40] In older adults, various factors can lead to reduced protein and total energy intake, increasing their susceptibility to disturbances in protein-energy balance, which contributes to loss of muscle mass.[41] mTORC1, which regulates muscle protein synthesis, senses plasma amino acids, glucose, and concentration of growth factors.[42] It initiates muscle protein synthesis only when both signaling pathways are sufficient. Essential amino acids, particularly leucine, are crucial for mTORC1 activation.[43] An adequate overall macronutrient balance is essential for proper functioning of the mTORC1 pathway, and the insulin-like growth factor 1 pathway, which regulate the anabolic-catabolic balance of tissues including skeletal muscle.[44,45] The anabolic resistance caused by biological changes underscores the need for a greater protein intake to maintain muscle homeostasis in older individuals.[46, 47]
Muscle protein is not maintained in a static state but is constantly in a dynamic balance between synthesis and breakdown, influenced by factors such as feeding, exercise, and fasting (Fig. 1).[48] Factors such as insulin resistance, chronic inflammation, systemic corticosteroid exposure, decreased growth or sex hormone levels related to aging or disease, and other factors, can affect this dynamic balance.[48] Ultimately, the net change in muscle mass is governed by the dynamics of muscle protein synthesis-breakdown mechanisms. Such changes can lead to anabolic resistance, where even resistance exercise and amino acid intake may not yield muscle protein synthesis rates comparable to those in young, healthy adults.[49]
In chronic and acute inflammation, specific cytokines (e.g., tumor necrosis factor-α, interleukin [IL]-1, IL-6), and systemic corticosteroid exposure can facilitate anabolic resistance and increase the expression of genes involved in muscle atrophy (atrogenes), such as Atrogin 1 and MURF1, which accelerate muscle protein breakdown.[50] Owing to the complex interactions and multiple factors contributing to the development of sarcopenia, distinguishing between primary sarcopenia associated with aging and secondary sarcopenia due to diseases such as tuberculosis and cancer, which expedite muscle protein breakdown, poses a significant challenge.[33] The involvement of these factors in the pathogenesis of sarcopenia has rendered them key targets for many new drug developments. For example, substances such as selective androgen receptor modulators (SARM) and exercise mimetics, were developed to promote muscle protein synthesis mechanisms.[51] Additionally, various drugs that block the myostatin-activin pathway, an upstream pathway of muscle atrophy, have been developed to inhibit muscle protein breakdown in situations of anabolic resistance.[52] Studies in humans have established clinical evidence showing that older adults and individuals with chronic diseases require greater protein intake to overcome anabolic resistance.[46]
The KWGS and AWGS 2019 guidelines recommend various methods for identifying sarcopenia.[7,10] Screening tools according to the KWGS guidelines are listed in Table 1. These methods include assessing calf circumference, hand grip strength, chair stand test, gait speed, and time up-and-go tests.[7,53-55] Additionally, questionnaires such as strength, assistance with walking, rising from a chair, climbing stairs, and falls (SARC-F) and ring tests using the thumb and index finger to measure calf circumference are suggested.[10,56] Notably, SARC-F has limitations as a screening tool due to its low sensitivity and high specificity.[57] Consequently, case identification in clinical practices may heavily rely on clinical suspicion, considering factors such as significant weight loss, general weakness, or history of falls, regardless of age. Clinical risk factors may include treatment affecting sex hormones, chronic use of glucocorticoids, chronic inflammatory conditions, and underlying malignancy.[10] Geriatric risks include mood, cognitive disorders, polypharmacy, chronic constipation, swallowing difficulties, falls, history of hospitalization, and other geriatric syndromes.[10]
Clinical assessment of sarcopenia fundamentally includes three essential elements: muscle mass, muscle strength, and physical function (Fig. 2). The KWGS and AWGS 2019 guidelines [7,10] defined sarcopenia as decreased muscle mass with low muscle strength or poor physical performance, and severe sarcopenia was classified as a state of decreased muscle mass with both weak muscle strength and decreased physical performance. The KWGS newly suggested the concept of functional sarcopenia as a state of weak muscle strength and low physical performance without a loss of muscle mass.[58]
The methods recommended for clinical use in Asia and Europe include dual energy X-ray absorptiometry (DXA) or bioimpedance analysis (BIA) to measure appendicular muscle mass.[6,7,10] The KWGS and AWGS 2019 advise adjusting the sum of the measured appendicular muscle mass by the square of the individual’s height (m2).[7,10] Meanwhile, the foundation for the NIH suggests adjusting by body mass index, which may be superior in predicting outcomes compared to height-squared adjustment.[5] The criteria for muscle mass reduction in the KWGS and AWGS 2019 are <7.0 kg/m2 for men and <5.4 kg/m2 for women in DXA, and <7.0 kg/m2 for men and <5.7 kg/m2 for women in BIA.
However, the measurement of lean mass through this indirect measurement methods (BIA and DXA) can lead to inconsistent associations with several outcomes, including immobility, disability, and falls.[9,59] Future evaluation of muscle quality using computed tomography and magnetic resonance imaging and direct measurement of muscle quantity using the D3-creatine dilution method may address this gap.[60]
The clinical assessment of muscle strength can be performed by measuring handgrip strength in the upper limbs or torque at the knee joint in the lower limbs. The KWGS and AWGS 2019 recommend muscle strength evaluation through a handgrip test. Handgrip measurements can be obtained using both spring-type (e.g., Smadley-type equipment) and hydraulic devices (e.g., Jamar’s equipment); however, the two methods have different measurement positions and may yield slightly different results.[61] The spring-type measurement is conducted with the elbow joint fully extended while standing; in cases where standing is not possible, the measurement can be done while sitting with the elbow joint fully extended.[62] The hydraulic measurement is performed with the elbow flexed at a 90-degree angle while sitting.[62] Although there is no standardized measurement protocol, it is generally recommended to take 2 to 3 measurements from each arm or dominant arm and select the best result from all measurements. The measurements generally do not have a time limit, and participants should be encouraged to exert maximum effort. In the KWGS and AWGS 2019, muscle strength <28 kg and <18 kg for men and women, respectively, is defined as muscle strength reduction.[7,10]
Physical function is a broad concept that includes muscle strength, physical activity, and other aspects such as patients’ reported outcomes. However, in the context of sarcopenia, quantitative assessment of whole-body motor performance through functional tests is considered a component of physical function. The most used and well-studied parameter that predicts outcomes is gait speed. The European guidelines define slow gait speed as <0.8 m/s when walking 4 m,[4] while the KWGS and AWGS 2019 define slow gait speed as <1.0 m/s when walking 6 m.[7,10]
The five-time chair rise test measures the duration to quickly rise from a chair with armrests without using arm support. The AWGS 2019 includes this item to categorize individuals who take >12 sec as having physical function impairment, while KWGS categorizes individuals who take >10 sec for the 5th stand and 11 sec for the 5th sit as physical function impairment.[7,10,63] The short physical performance battery consists of three items: static balance assessment, gait speed, and five-time chair rise test.[64] It is calculated on a scale of 0 to 12 points and is used as a tool for evaluating physical function. The KWGS and AWGS 2019 guidelines categorize individuals with a score of 9 or lower as having physical function impairment.[7,10]
As sarcopenia is a geriatric syndrome affected by the combinations of multiple biological and functional issues, its multifaceted characteristics require a patient-centered clinical approach (Fig. 3). The pattern of correctable pathophysiology may differ vastly among individuals in actual clinical practice. Patient-centered approach in the manner of comprehensive geriatric assessment (CGA) or briefer approaches such as the Integrated Care for Older People can be crucial in establishing an individualized care plan.[65,66] These assessment can help identify issues related to activities of daily living, cognition, mood, nutrition, social support, and other aspects.[67] Therefore, the KWGS guideline highlights the execution of CGA after the diagnosis of sarcopenia.[10] Assessing the management of chronic diseases and examining the medications administered are also necessary. The general approach on the underlying factors related to muscle loss and functional decline in patients involves basic clinical strategies similar to those for weight loss or frailty in the context of aging, including medical assessments for myriads of secondary causes that may entail malignancies, inflammatory conditions, infections, cardiopulmonary, hepatic, nephrologic, endocrinological conditions, neurological, and musculoskeletal conditions.
In clinical settings, the foundation for developing a treatment plan for sarcopenia lies in correcting the identified contributing factors through individualized approaches for patients. While nutritional and exercise interventions, as well as addressing underlying conditions and contributing factors, are crucial, no pharmacological agents have been definitively proven to have a significant impact on sarcopenia. Multifaceted interventions, including resistance exercises, have been validated to improve physical function in various population groups.[30,68] It remains unclear whether such interventions are cost-effective from a population perspective, thus emphasizing the need for further research. The International Clinical Practice Guidelines for Sarcopenia by the ICFSR indicate that exercise is supported by strong evidence and moderate certainty, while protein intake has moderate evidence strength with low certainty.[69] However, there is little evidence that vitamin D, hormones, or new medications can aid with sarcopenia management.
Physical activity, with a focus on progressive strength training, is recognized as the primary treatment for sarcopenia. While most of the studies on effective exercise intervention studies have not targeted older populations diagnosed with sarcopenia, structured exercise may potentially improve parameters such as muscle strength, walking speed, and simple physical function in populations with concurrent sarcopenia.[30,36] Additionally, further studies are warranted to ascertain how exercise can prevent disability and maintain activities of daily living. Exercise programs aimed at improving accessibility in the metaverse have been explored recently; however, additional validation studies are required for further assessment.[70]
The recommendations for protein intake to counteract anabolic resistance are primarily rooted in studies that incorporate amino acids, an approach that analyzes the rate of incorporation of administered exogenous amino acids into muscle proteins during anabolic resistance.[71] Individual studies continue to report that protein supplementation can improve physical function in older populations where malnutrition or weight loss is observed.[72] Whether protein intake can improve patient-reported outcomes in patients with sarcopenia patients and whether it is cost-effective requires well-designed clinical studies. Experts generally recommend a slightly higher protein intake of 1.2 to 1.5 g/kg/day instead of the recommended dietary allowance of 0.9 g/kg/day to overcome anabolic resistance associated with aging.[47,73] Branched-chain amino acids and their metabolite leucine and β-hydroxy-beta-methylbutyrate have the potential for enhancing muscle protein synthesis but require more extensive clinical recommendations for the overall populations with sarcopenia.[74,75] Vitamin D has been studied extensively in relation to sarcopenia, and while observational studies show associations between sarcopenia and vitamin D deficiency, clinical evidence for vitamin D supplementation improving physical function or muscle mass is insufficient.[76]
Several targeted drug development approaches for sarcopenia are ongoing. Myostatin (GDF-8) is a highly researched substance in the context of drug development for diseases characterized by muscle loss. Myostatin is expressed in muscle cells and binds to activin receptors (ACVR2B), increasing the expression of genes related to muscle atrophy and suppressing those involved in muscle cell growth and differentiation.[77] In animal models, genetic inhibition of myostatin increases muscle function,[78] and this effect has been reported in humans.[79] Several drugs, such as Stamulumab, Landogrozumab (LY-2495655), Trevogrumab (REGN1033), and Bimagrumab (BYM388), which target the myostatin-activin pathway, have been developed, and multiple clinical trials have been conducted. While some studies report a significant increase in muscle mass,[80] no clinical research has demonstrated a significant improvement in physical function. Exercise mimetics are substances that activate beneficial metabolic pathways in a similar manner to exercise. One example is GW1516, a peroxisome proliferator-activated receptor-β/δ agonist that enhances exercise capacity in animal experiments.[81] However, evidence of its use in humans remain limited, and is currently considered a banned substance for international athletes. AMP-activated protein kinase (AMPK) activators such as 5-aminoimidazole-4-carboxamide ribonucleotide (AICAR) and metformin have shown potential in animal studies but lack sufficient clinical evidence.[82] SARMs such as enobosarm (MK-2866) [83] and PF-05314882 [84] have been developed, with preliminary clinical trial results showing improvements in muscle mass and physical function. However, robust evidence for their use in sarcopenia remains lacking.
Sarcopenia, a common geriatric syndrome in older adults, is associated with poor outcomes in various clinical settings, necessitating both prevention and intervention. Complex pathophysiological changes related to aging are believed to impact muscle mass and function, and a multi-faceted approach, centered on exercise and nutrition, can prevent progression, and improve physical function. In clinical practice, an individualized approach that is patient-centered and rectifies identified contributing factors is essential. Although there are no treatment options for sarcopenia, that definitively improve quality of life and physical function, ongoing drug development research is expected to lead to the development of therapeutic strategies for this condition, increasing clinical applications in the future.
Fig. 1
Abbreviated mechanism of muscle protein synthesis and breakdown. mTORC1, mechanistic target of rapamycin complex 1; S6K, S6 kinase; 4EBP1, eIF4E-binding protein; UPS, ubiquitin-proteasome system.
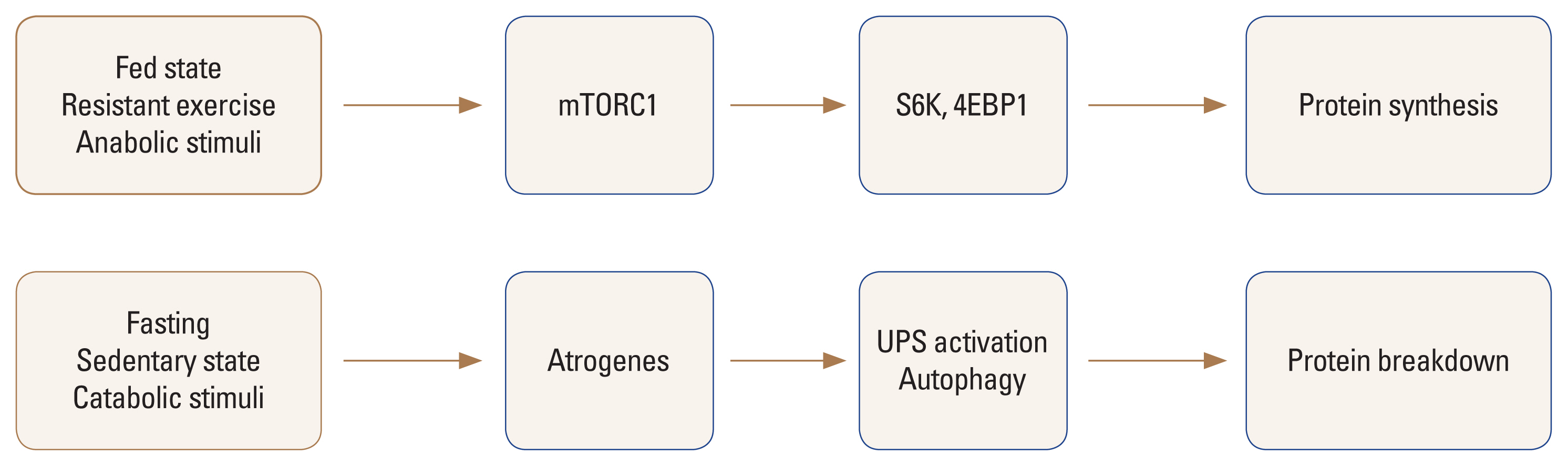
Fig. 2
Confirmatory tests for sarcopenia evaluation based on the Korean Working Group on Sarcopenia (KWGS) guideline. SPPB, short physical performance battery; M, male; F, female; ASM, appendicular skeletal muscle mass; DXA, dual energy X-ray absorptiometry (KWGS guideline); BIA, bioimpedance analysis.
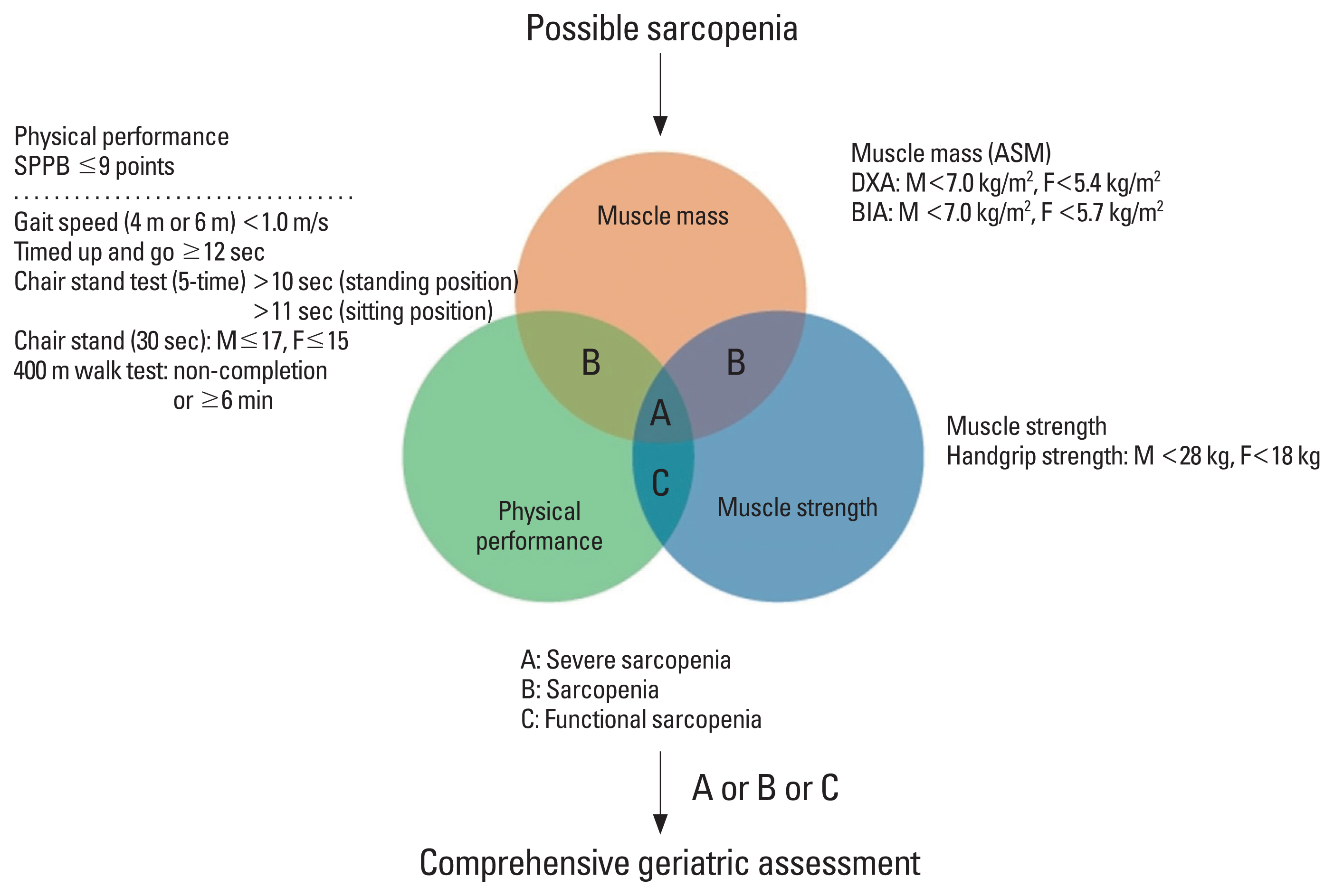
Fig. 3
Sarcopenia as a complexed system consisting of multiple pathophysiology in both biological and clinical aspects (adapted from the Korean Working Group on Sarcopenia guideline). ADL, activities for daily living; IADL, instrumental activities of daily living.
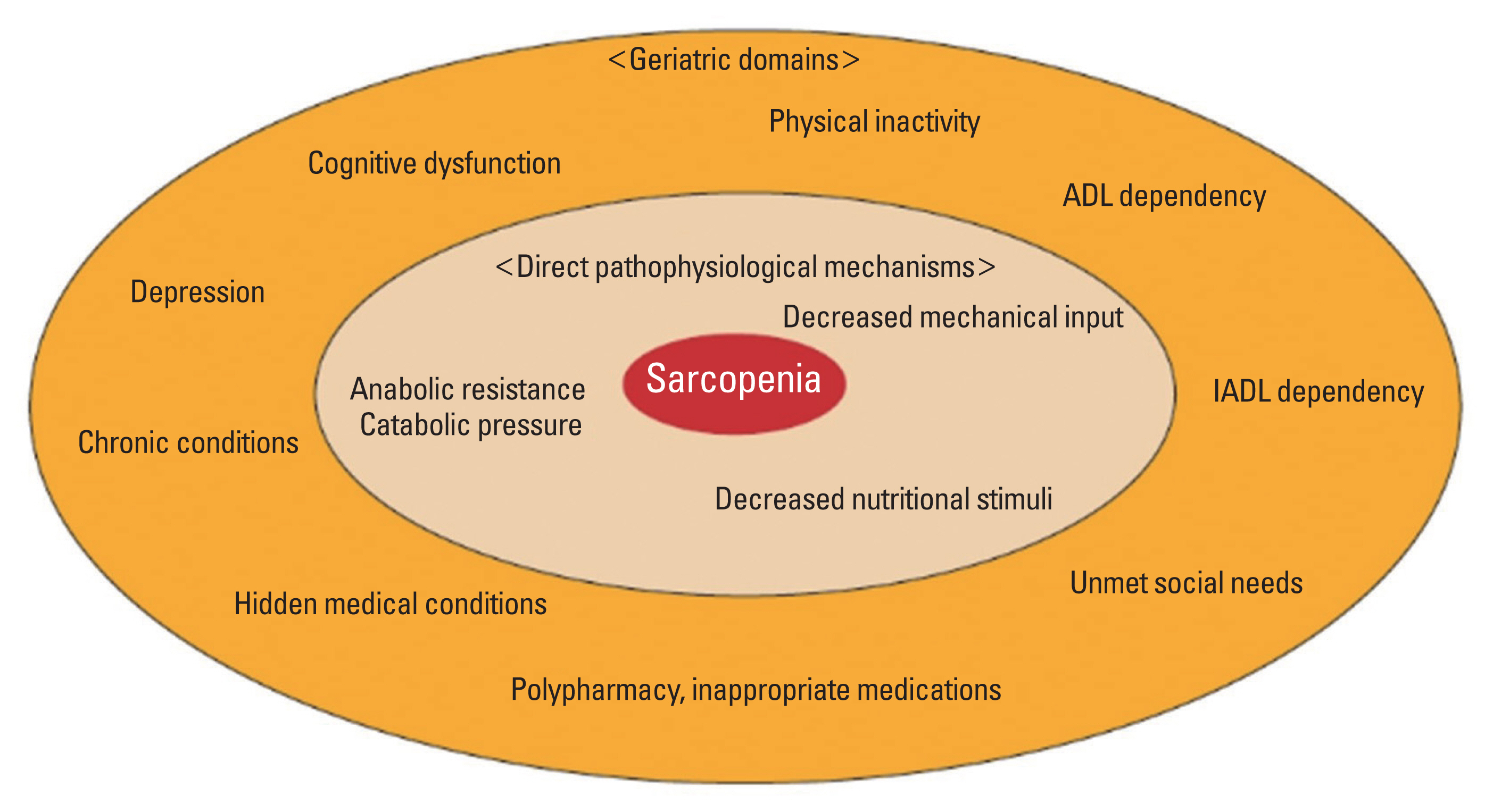
Table 1
Screening tests for sarcopenia (adapted from the Korean Working Group on Sarcopenia guideline)
| Tools | Cut-offs | References |
|---|---|---|
| SARC-F | ≥4 | Chen et al. [7] |
|
|
||
| Calf circumference | Male: <34 cm | Chen et al. [7] |
| Female: <33 cm | ||
|
|
||
| Chair stand test | ||
| 5-time | Standing position: >10 sec | Yamada et al. [54] |
| Sitting position: >11 sec | ||
| 30 seconds | Male: <17 | Sawada et al. [53] |
| Female: <15 | ||
|
|
||
| Handgrip strength | Male: <28 kg | Chen et al. [7] |
| Female: <18 kg | ||
|
|
||
| Gait speed (4 m or 6 m) | <1 m/s | Chen et al. [7] |
|
|
||
| Timed up and go test | ≥12 sec | Jung et al. [55] |
REFERENCES
1. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019;393:2636-46.
https://doi.org/10.1016/s0140-6736(19)31138-9.


2. Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 1998;147:755-63.
https://doi.org/10.1093/oxfordjournals.aje.a009520.


3. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 2002;50:889-96.
https://doi.org/10.1046/j.1532-5415.2002.50216.x.


4. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing 2010;39:412-23.
https://doi.org/10.1093/ageing/afq034.



5. Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 2014;69:547-58.
https://doi.org/10.1093/gerona/glu010.



6. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16-31.
https://doi.org/10.1093/ageing/afy169.



7. Chen LK, Woo J, Assantachai P, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020;21:300-7e2..
https://doi.org/10.1016/j.jamda.2019.12.012.


8. Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc 2014;15:95-101.
https://doi.org/10.1016/j.jamda.2013.11.025.


9. Reginster JY, Beaudart C, Al-Daghri N, et al. Update on the ESCEO recommendation for the conduct of clinical trials for drugs aiming at the treatment of sarcopenia in older adults. Aging Clin Exp Res 2021;33:3-17.
https://doi.org/10.1007/s40520-020-01663-4.



10. Baek JY, Jung HW, Kim KM, et al. Korean working group on sarcopenia guideline: expert consensus on sarcopenia screening and diagnosis by the Korean Society of Sarcopenia, the Korean Society for Bone and Mineral Research, and the Korean Geriatrics Society. Ann Geriatr Med Res 2023;27:9-21.
https://doi.org/10.4235/agmr.23.0009.



11. Jung HW, Baek JY. New clinical practice guidelines for sarcopenia screening and diagnosis in Korean older adults: a step forward. Ann Geriatr Med Res 2023;27:1-2.
https://doi.org/10.4235/agmr.23.0033.



12. Cruz-Jentoft AJ, Landi F, Topinková E, et al. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care 2010;13:1-7.
https://doi.org/10.1097/MCO.0b013e328333c1c1.


13. Bernabei R, Martone AM, Vetrano DL, et al. Frailty, physical frailty, sarcopenia: a new conceptual model. Stud Health Technol Inform 2014;203:78-84.

14. Cesari M, Landi F, Vellas B, et al. Sarcopenia and physical frailty: two sides of the same coin. Front Aging Neurosci 2014;6:192.
https://doi.org/10.3389/fnagi.2014.00192.



15. Schaap LA, van Schoor NM, Lips P, et al. Associations of sarcopenia definitions, and their components, with the incidence of recurrent falling and fractures: the longitudinal aging study Amsterdam. J Gerontol A Biol Sci Med Sci 2018;73:1199-204.
https://doi.org/10.1093/gerona/glx245.


16. Steffl M, Bohannon RW, Sontakova L, et al. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging 2017;12:835-45.
https://doi.org/10.2147/cia.S132940.



17. Jang IY, Lee E, Lee H, et al. Characteristics of sarcopenia by European consensuses and a phenotype score. J Cachexia Sarcopenia Muscle 2020;11:497-504.
https://doi.org/10.1002/jcsm.12507.



18. Anker SD, Morley JE, von Haehling S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle 2016;7:512-4.
https://doi.org/10.1002/jcsm.12147.



19. Evans WJ, Guralnik J, Cawthon P, et al. Sarcopenia: no consensus, no diagnostic criteria, and no approved indication-How did we get here? Geroscience 2024;46:183-90.
https://doi.org/10.1007/s11357-023-01016-9.



20. Baek JY, Lee E, Jung HW, et al. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res 2021;25:65-71.
https://doi.org/10.4235/agmr.21.0063.



21. Kim M, Won CW. Sarcopenia in Korean community-dwelling adults aged 70 years and older: application of screening and diagnostic tools from the Asian working group for sarcopenia 2019 update. J Am Med Dir Assoc 2020;21:752-8.
https://doi.org/10.1016/j.jamda.2020.03.018.


22. Kim M, Won CW. Prevalence of sarcopenia in community-dwelling older adults using the definition of the European Working Group on Sarcopenia in Older People 2: findings from the Korean Frailty and Aging Cohort Study. Age Ageing 2019;48:910-6.
https://doi.org/10.1093/ageing/afz091.


23. Lim S, Kim JH, Yoon JW, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care 2010;33:1652-4.
https://doi.org/10.2337/dc10-0107.



24. Yigit B, Oner C, Cetin H, et al. Association between sarcopenia and cognitive functions in older individuals: a cross-sectional study. Ann Geriatr Med Res 2022;26:134-9.
https://doi.org/10.4235/agmr.22.0027.



25. Bunout D, de la Maza MP, Barrera G, et al. Association between sarcopenia and mortality in healthy older people. Australas J Ageing 2011;30:89-92.
https://doi.org/10.1111/j.1741-6612.2010.00448.x.


26. Cacciatore S, Massaro C, Landi F. Preventing osteoporosis, sarcopenia and obesity to care about quality of life. Ann Geriatr Med Res 2023;27:87-90.
https://doi.org/10.4235/agmr.22.0158.



27. Hossain M, Yu D, Bikdeli B, et al. Sarcopenia and adverse post-surgical outcomes in geriatric patients: a scoping review. J Frailty Aging 2021;10:63-9.
https://doi.org/10.14283/jfa.2020.27.


28. Davis MP, Panikkar R. Sarcopenia associated with chemotherapy and targeted agents for cancer therapy. Ann Palliat Med 2019;8:86-101.
https://doi.org/10.21037/apm.2018.08.02.


29. Kim TN, Choi KM. Sarcopenia: definition, epidemiology, and pathophysiology. J Bone Metab 2013;20:1-10.
https://doi.org/10.11005/jbm.2013.20.1.1.



30. Shen Y, Shi Q, Nong K, et al. Exercise for sarcopenia in older people: a systematic review and network meta-analysis. J Cachexia Sarcopenia Muscle 2023;14:1199-211.
https://doi.org/10.1002/jcsm.13225.



31. Moreira-Pais A, Ferreira R, Oliveira PA, et al. A neuromuscular perspective of sarcopenia pathogenesis: deciphering the signaling pathways involved. Geroscience 2022;44:1199-213.
https://doi.org/10.1007/s11357-021-00510-2.



32. Peter AK, Cheng H, Ross RS, et al. The costamere bridges sarcomeres to the sarcolemma in striated muscle. Prog Pediatr Cardiol 2011;31:83-8.
https://doi.org/10.1016/j.ppedcard.2011.02.003.



33. Sartori R, Romanello V, Sandri M. Mechanisms of muscle atrophy and hypertrophy: implications in health and disease. Nat Commun 2021;12:330.
https://doi.org/10.1038/s41467-020-20123-1.



34. Phillips SM, Tipton KD, Aarsland A, et al. Mixed muscle protein synthesis and breakdown after resistance exercise in humans. Am J Physiol 1997;273:E99-107.
https://doi.org/10.1152/ajpendo.1997.273.1.E99.


35. Gasier HG, Fluckey JD, Previs SF, et al. Acute resistance exercise augments integrative myofibrillar protein synthesis. Metabolism 2012;61:153-6.
https://doi.org/10.1016/j.metabol.2011.07.001.


36. Kim DY, Oh SL, Lim JY. Applications of eccentric exercise to improve muscle and mobility function in older adults. Ann Geriatr Med Res 2022;26:4-15.
https://doi.org/10.4235/agmr.21.0138.



37. Ziaaldini MM, Marzetti E, Picca A, et al. Biochemical pathways of sarcopenia and their modulation by physical exercise: a narrative review. Front Med (Lausanne) 2017;4:167.
https://doi.org/10.3389/fmed.2017.00167.



38. Deschenes MR, Flannery R, Hawbaker A, et al. Adaptive remodeling of the neuromuscular junction with aging. Cells 2022;11:1150.
https://doi.org/10.3390/cells11071150.



39. Kortebein P, Symons TB, Ferrando A, et al. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol A Biol Sci Med Sci 2008;63:1076-81.
https://doi.org/10.1093/gerona/63.10.1076.


40. Robinson S, Cooper C, Aihie Sayer A. Nutrition and sarcopenia: a review of the evidence and implications for preventive strategies. J Aging Res 2012;2012:510801.
https://doi.org/10.1155/2012/510801.



41. Norman K, Haß U, Pirlich M. Malnutrition in older adults-recent advances and remaining challenges. Nutrients 2021;13:2764.
https://doi.org/10.3390/nu13082764.



42. Yoon MS. mTOR as a key regulator in maintaining skeletal muscle mass. Front Physiol 2017;8:788.
https://doi.org/10.3389/fphys.2017.00788.



43. Zhao Y, Cholewa J, Shang H, et al. Advances in the role of leucine-sensing in the regulation of protein synthesis in aging skeletal muscle. Front Cell Dev Biol 2021;9:646482.
https://doi.org/10.3389/fcell.2021.646482.



44. Adams GR, Haddad F. The relationships among IGF-1, DNA content, and protein accumulation during skeletal muscle hypertrophy. J Appl Physiol (1985) 1996;81:2509-16.
https://doi.org/10.1152/jappl.1996.81.6.2509.


45. Cuthbertson D, Smith K, Babraj J, et al. Anabolic signaling deficits underlie amino acid resistance of wasting, aging muscle. FASEB J 2005;19:422-4.
https://doi.org/10.1096/fj.04-2640fje.


46. Haran PH, Rivas DA, Fielding RA. Role and potential mechanisms of anabolic resistance in sarcopenia. J Cachexia Sarcopenia Muscle 2012;3:157-62.
https://doi.org/10.1007/s13539-012-0068-4.



47. Jung HW, Kim SW, Kim IY, et al. Protein intake recommendation for Korean older adults to prevent sarcopenia: expert consensus by the Korean geriatric society and the Korean nutrition society. Ann Geriatr Med Res 2018;22:167-75.
https://doi.org/10.4235/agmr.18.0046.



48. Tipton KD, Hamilton DL, Gallagher IJ. Assessing the role of muscle protein breakdown in response to nutrition and exercise in humans. Sports Med 2018;48:53-64.
https://doi.org/10.1007/s40279-017-0845-5.



49. Burd NA, Gorissen SH, van Loon LJ. Anabolic resistance of muscle protein synthesis with aging. Exerc Sport Sci Rev 2013;41:169-73.
https://doi.org/10.1097/JES.0b013e318292f3d5.


50. Draganidis D, Jamurtas AZ, Chondrogianni N, et al. Low-grade systemic inflammation interferes with anabolic and catabolic characteristics of the aged human skeletal muscle. Oxid Med Cell Longev 2021;2021:8376915.
https://doi.org/10.1155/2021/8376915.



51. Christiansen AR, Lipshultz LI, Hotaling JM, et al. Selective androgen receptor modulators: the future of androgen therapy? Transl Androl Urol 2020;9:S135-48.
https://doi.org/10.21037/tau.2019.11.02.



52. Kim BJ. Effects of muscles on bone metabolism-with a focus on myokines. Ann Geriatr Med Res 2022;26:63-71.
https://doi.org/10.4235/agmr.22.0054.



53. Sawada S, Ozaki H, Natsume T, et al. The 30-s chair stand test can be a useful tool for screening sarcopenia in elderly Japanese participants. BMC Musculoskelet Disord 2021;22:639.
https://doi.org/10.1186/s12891-021-04524-x.



54. Yamada M, Lim JY, Assantachai P, et al. Five-repetition sit-to-stand test: end with the fifth stand or sit? Geriatr Gerontol Int 2022;22:362-4.
https://doi.org/10.1111/ggi.14358.


55. Jung HW, Kim S, Jang IY, et al. Screening value of timed up and go test for frailty and low physical performance in Korean older population: the Korean frailty and aging cohort study (KFACS). Ann Geriatr Med Res 2020;24:259-66.
https://doi.org/10.4235/agmr.20.0072.



56. Rose Berlin Piodena-Aportadera M, Lau S, Chew J, et al. Calf circumference measurement protocols for sarcopenia screening: differences in agreement, convergent validity and diagnostic performance. Ann Geriatr Med Res 2022;26:215-24.
https://doi.org/10.4235/agmr.22.0057.



57. Lim JY, Low NA, Merchant RA. Prevalence of sarcopenia in pre-frail community dwelling older adult and utility of SARC-F, SARC-CalF and calf circumference in case finding. J Frailty Sarcopenia Falls 2020;5:53-6.
https://doi.org/10.22540/jfsf-05-053.



58. Ji S, Baek JY, Lee E, et al. Phenotype validation of the Korean working group on sarcopenia guideline. Arch Gerontol Geriatr 2024;117:105251.
https://doi.org/10.1016/j.archger.2023.105251.


59. Lunt E, Ong T, Gordon AL, et al. The clinical usefulness of muscle mass and strength measures in older people: A systematic review. age Ageing 2021;50:88-95.
https://doi.org/10.1093/ageing/afaa123.



60. Evans WJ, Hellerstein M, Orwoll E, et al. D(3)-Creatine dilution and the importance of accuracy in the assessment of skeletal muscle mass. J Cachexia Sarcopenia Muscle 2019;10:14-21.
https://doi.org/10.1002/jcsm.12390.



61. Kim M, Shinkai S. Prevalence of muscle weakness based on different diagnostic criteria in community-dwelling older adults: a comparison of grip strength dynamometers. Geriatr Gerontol Int 2017;17:2089-95.
https://doi.org/10.1111/ggi.13027.


62. Roberts HC, Denison HJ, Martin HJ, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011;40:423-9.
https://doi.org/10.1093/ageing/afr051.


63. Ji S, Jang R, Roh H, et al. Comparing chair stand test protocols: fifth stand versus fifth sit. Geriatr Gerontol Int 2023;23:976-8.
https://doi.org/10.1111/ggi.14723.


64. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85-94.
https://doi.org/10.1093/geronj/49.2.m85.


65. Jung HW. Visualizing domains of comprehensive geriatric assessments to grasp frailty spectrum in older adults with a radar chart. Ann Geriatr Med Res 2020;24:55-6.
https://doi.org/10.4235/agmr.20.0013.



66. Tavassoli N, de Souto Barreto P, Berbon C, et al. Implementation of the WHO integrated care for older people (ICOPE) programme in clinical practice: a prospective study. Lancet Healthy Longev 2022;3:e394-e404.
https://doi.org/10.1016/s2666-7568(22)00097-6.


67. Wong HJ, Harith S, Lua PL, et al. Possible sarcopenia and its association with nutritional status, dietary intakes, physical activity and health-related quality of life among older stroke survivors. Ann Geriatr Med Res 2022;26:162-74.
https://doi.org/10.4235/agmr.22.0033.



68. Oh G, Lee H, Park CM, et al. Long-term effect of a 24-week multicomponent intervention on physical performance and frailty in community-dwelling older adults. Age Ageing 2021;50:2157-66.
https://doi.org/10.1093/ageing/afab149.



69. Dent E, Morley JE, Cruz-Jentoft AJ, et al. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 2018;22:1148-61.
https://doi.org/10.1007/s12603-018-1139-9.


70. Park TS, Shin MJ. Effectiveness of an exercise program for older adults using an augmented reality exercise platform: a pilot study. Ann Geriatr Med Res 2023;27:73-9.
https://doi.org/10.4235/agmr.23.0016.



71. Paulussen KJM, McKenna CF, Beals JW, et al. Anabolic resistance of muscle protein turnover comes in various shapes and sizes. Front Nutr 2021;8:615849.
https://doi.org/10.3389/fnut.2021.615849.



72. Cintineo HP, Arent MA, Antonio J, et al. Effects of protein supplementation on performance and recovery in resistance and endurance training. Front Nutr 2018;5:83.
https://doi.org/10.3389/fnut.2018.00083.



73. Rogeri PS, Zanella R Jr, Martins GL, et al. Strategies to prevent sarcopenia in the aging process: role of protein intake and exercise. Nutrients 2021;14:52.
https://doi.org/10.3390/nu14010052.



74. Ko CH, Wu SJ, Wang ST, et al. Effects of enriched branched-chain amino acid supplementation on sarcopenia. Aging (Albany NY) 2020;12:15091-103.
https://doi.org/10.18632/aging.103576.



75. Oktaviana J, Zanker J, Vogrin S, et al. The effect of β-hydroxy-β-methylbutyrate (HMB) on sarcopenia and functional frailty in older persons: a systematic review. J Nutr Health Aging 2019;23:145-50.
https://doi.org/10.1007/s12603-018-1153-y.


76. Uchitomi R, Oyabu M, Kamei Y. Vitamin D and sarcopenia: Potential of vitamin D supplementation in sarcopenia prevention and treatment. Nutrients 2020;12:3189.
https://doi.org/10.3390/nu12103189.



77. McPherron AC, Lee SJ. Double muscling in cattle due to mutations in the myostatin gene. Proc Natl Acad Sci U S A 1997;94:12457-61.
https://doi.org/10.1073/pnas.94.23.12457.



78. Bogdanovich S, Krag TO, Barton ER, et al. Functional improvement of dystrophic muscle by myostatin blockade. Nature 2002;420:418-21.
https://doi.org/10.1038/nature01154.


79. Schuelke M, Wagner KR, Stolz LE, et al. Myostatin mutation associated with gross muscle hypertrophy in a child. N Engl J Med 2004;350:2682-8.
https://doi.org/10.1056/NEJMoa040933.


80. Becker C, Lord SR, Studenski SA, et al. Myostatin antibody (LY2495655) in older weak fallers: a proof-of-concept, randomised, phase 2 trial. Lancet Diabetes Endocrinol 2015;3:948-57.
https://doi.org/10.1016/s2213-8587(15)00298-3.


81. Narkar VA, Downes M, Yu RT, et al. AMPK and PPARdelta agonists are exercise mimetics. Cell 2008;134:405-15.
https://doi.org/10.1016/j.cell.2008.06.051.



82. Mohammed I, Hollenberg MD, Ding H, et al. A critical review of the evidence that metformin is a putative anti-aging drug that enhances healthspan and extends lifespan. Front Endocrinol (Lausanne) 2021;12:718942.
https://doi.org/10.3389/fendo.2021.718942.



83. Dalton JT, Barnette KG, Bohl CE, et al. The selective androgen receptor modulator GTx-024 (enobosarm) improves lean body mass and physical function in healthy elderly men and postmenopausal women: results of a double-blind, placebo-controlled phase II trial. J Cachexia Sarcopenia Muscle 2011;2:153-61.
https://doi.org/10.1007/s13539-011-0034-6.



84. Papanicolaou DA, Ather SN, Zhu H, et al. A phase IIA randomized, placebo-controlled clinical trial to study the efficacy and safety of the selective androgen receptor modulator (SARM), MK-0773 in female participants with sarcopenia. J Nutr Health Aging 2013;17:533-43.
https://doi.org/10.1007/s12603-013-0335-x.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 2,202 View
- 71 Download
- ORCID iDs
-
Sunghwan Ji

https://orcid.org/0000-0002-8150-933XHee-Won Jung

https://orcid.org/0000-0002-2583-3354Ji Yeon Baek

https://orcid.org/0000-0001-7547-8015Il-Young Jang

https://orcid.org/0000-0003-3617-3301Eunju Lee

https://orcid.org/0000-0003-4612-0625 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



