 |
 |
| jbm > Volume 30(4); 2023 > Article |
|
Abstract
Orthodontic tooth movement (OTM) is achieved by the simultaneous activation of bone resorption by osteoclasts and bone formation by osteoblasts. When orthodontic forces are applied, osteoclast-mediated bone resorption occurs in the alveolar bone on the compression side, creating space for tooth movement. Therefore, controlling osteoclastogenesis is the fundamental tenet of orthodontic treatment. Orthodontic forces are sensed by osteoblast lineage cells such as periodontal ligament (PDL) cells and osteocytes. Of several cytokines produced by these cells, the most important cytokine promoting osteoclastogenesis is the receptor activator of nuclear factor-κB ligand (RANKL), which is mainly supplied by osteoblasts. Additionally, osteocytes embedded within the bone matrix, T lymphocytes in inflammatory conditions, and PDL cells produce RANKL. Besides RANKL, inflammatory cytokines, such as interleukin-1, tumor necrosis factor-α, and prostaglandin E2 promote osteoclastogenesis under OTM. On the downside, excessive osteoclastogenesis activation triggers orthodontically-induced external root resorption (ERR) through pro-osteoclastic inflammatory cytokines. Therefore, understanding the mechanisms of osteoclastogenesis during OTM is essential in reducing the adverse effects of orthodontic treatment. Here, we review the current concepts of the mechanisms underlying osteoclastogenesis in OTM and orthodontically induced ERR.
Orthodontic tooth movement (OTM) is the process by which orthodontic force — mechanical force deliberately delivered by orthodontic appliances — causes the tooth to move within the alveolar bone due to an accelerated bone remodeling process. The tooth is attached to the alveolar bone through the periodontium, which consists of several units of mineralized and non-mineralized tissues, such as the cementum on the tooth root surface, the periodontal ligament (PDL), the alveolar bone, and the gingiva.[1] The PDL is a dense connective tissue that plays a critical role in supporting the tooth within its socket. It comprises various components, including bundles of collagenous fibers primarily composed of type I collagen. The Sharpey’s fibers are the terminal segment of the PDL that insert into the cementum and the alveolar bone on each side. They are aligned in different orientations across different locations to anchor the tooth to the surrounding alveolar bone. The cementum is a thin mineralized tissue layer covering the tooth root. The integrity of the cementum is important for tooth stability and protecting the tooth from external resorption.[2] The alveolar bone is a mineralized tissue that undergoes a finely controlled process, coordinating bone resorption by osteoclasts and bone formation by osteoblasts.[3] It has a high rate of bone turnover compared to the axial and appendicular skeleton.[4,5] One unique aspect of the alveolar bone is that it is of the neural crest origin.[6] Orthodontic force is transmitted from the tooth to the alveolar bone through the surrounding PDL, resulting in reversible micro-injuries of the PDL. This triggers the movement of the teeth within the alveolar bone. During the initial application of orthodontic force, the tooth moves within the PDL space, causing the PDL to either stretch or compress. On the tension side where PDL is stretched, osteoblastic activities are enhanced, which results in osteoid deposition, mineralization, and eventually new bone formation. On the compression side, bone resorption occurs through the activation of osteoclasts via a sterile inflammatory response triggered by proinflammatory cytokines.[7] These proinflammatory cytokines contribute to bone resorption by inducing the expression of a receptor activator of nuclear factor (NF)-κB ligand (RANKL), a member of the tumor necrosis factor (TNF) family. RANKL binds to its receptor RANK to induce osteoclastogenesis.[8,9] Excessive compressive force generated by orthodontic force can also stimulate a significant increase in RANKL expression in periodontal tissues, potentially leading to the pathological resorption of the cementum termed orthodontically induced external root resorption (ERR). ERR is irreversible when the resorption involves the dentin.[10,11]
Malocclusion is one of the most common dentoalveolar anomalies that impair oral function and craniofacial growth, typically associated with the impairment in breathing, chewing, speaking, and facial appearance. Therefore, the demand for orthodontic treatment is strong. However, orthodontic treatment is a lengthy process, typically spanning over 2 years with an inherent risk for tooth root resorption. Therefore, it is crucial to have better understanding of the fundamental biological mechanisms of OTM and orthodontically induced ERR to ameliorate risks associated with orthodontic treatment. This review summarizes the current concept of the mechanisms of osteoclastogenesis during OTM and orthodontically induced ERR.
RANKL, a member of the TNF family, is an essential cytokine for osteoclastogenesis.[8,9] RANKL binds to its receptor RANK, which is expressed on osteoclast precursor cells, to induce osteoclastogenesis through the activation of transcription factors, such as the NF of activated T cells 1 (NFATc1).[12] The importance of RANKL in bone metabolism in vivo has been demonstrated by studies of RANKL-knockout (KO) mice. RANKL- and RANK-KO mice show osteopetrosis with a complete absence of osteoclasts.[9] In addition, RANKL-KO mice are protected from bone erosion during arthritis, demonstrating that osteoclastogenesis under inflammatory conditions is dependent on RANKL.[13] Among the cells constituting the periodontal tissues, it has been reported that RANKL is expressed by PDL cells, osteoblasts, osteocytes, and T lymphocytes.[3,14-17] The RANKL-RANK pathway critically contributes to OTM, as many osteoclasts are observed on the compression side of the tooth in a sterile inflammatory condition induced by orthodontic forces. In fact, the administration of anti-RANKL antibodies delays OTM.[14] Therefore, efforts have been made to elucidate which cellular source of RANKL in periodontal tissues is important for OTM (Fig. 1, Table 1).
One clinically important observation is that temporary anchorage devices, which are widely used as an orthodontic anchorage, or ankylosed teeth, which are fused to alveolar bones, don’t move even with the persistent application of orthodontic force.[18] This has led to the theory that PDL cells may serve as a primary source of RANKL in OTM. Ogasawara et al. [17] show RANKL expression in periodontal tissues by in situ hybridization, reporting that osteoblasts and PDL cells express Tnfsf11 (encoding RANKL) mRNAs under physiological conditions. During OTM, RANKL-positive PDL cells increase on the compression side. Functionally, RANKL deletion in osteoblasts and PDL cells using a tamoxifen-inducible 3.2 kb collagen1α1 promoter creER (3.2 kb Col1a1-creER) transgenic line blocks OTM.[19] Therefore, osteoblasts and PDL cells are an important source of RANKL in OTM.
Factors supporting the formation of PDL are involved in regulating RANKL expression. The transcription factor mohawk homeobox (Mkx) plays an important role in tendon maturation by regulating the expression of type I collagen. Mkx is also expressed in the PDL and is responsible for periodontal tissue homeostasis by suppressing the differentiation of PDL cells into osteoblasts.[20] In Mkx-KO rats, OTM was suppressed through a decline in RANKL expression in PDL cells.[16] Another important molecule, periostin, is a secreted extracellular matrix protein highly expressed in PDL and periosteum, regulating periodontal tissue homeostasis. Periostin-KO mice showed a reduced number of RANKL-positive stromal cells and osteoclasts on the compression side, consequently inhibiting OTM.[21]
Osteocytes account for about 90% of the cells that make up bone and are by far the largest in number among bone-constituent cells. Two comprehensive genetic engineering studies show that RANKL deletion by Dmp1-cre, which marks a majority of osteocytes, reduces the number of osteoclasts during the adult stage.[22,23] These studies show the primary source of RANKL under physiological conditions in adult stages is predominantly osteocytes.
Osteocytes extend their dendrite-like projections in the bone matrix and are in close contact with other osteocytes. This osteocyte network is thought to regulate bone homeostasis by enabling the sensing and response to mechanical stimuli transmitted through bone.[24,25] Therefore, it is postulated that osteocytes respond to orthodontic forces and are involved in OTM. In the osteocyte-ablated model using the diphtheria toxin receptor-mediated cell ablation system under the control of a Dmp1 promoter, there is a decrease in the number of osteoclasts on the compression side and a delay in OTM.[26] Additionally, Shoji-Matsunaga et al. [14] demonstrate that the number of osteoclasts on the compression side are reduced when OTM is induced in mice in which RANKL is ablated by Dmp1-cre. However, Dmp1-cre has been shown to be active in cell types other than osteocytes.[27-29] Therefore, experiments with a truly osteocyte-specific cre line is needed to definitively support the above-described osteocyte-centric notion on OTM. More specifically, the source of RANKL in OTM should be clarified in future studies.
Surgical techniques, such as corticotomy, are widely applied in orthodontic practice to accelerate orthodontic treatment.[30] It is speculated that this intervention induces an accumulation of immune cells due to corticotomy-induced bone damage, which speeds up OTM.[31] Immune cells located in the gingiva and PDL contribute to osteoclastogenesis.[32] For example, OTM is delayed in nude mice lacking mature T cells.[33] When T cells are transplanted into these mice, OTM is accelerated associated with increased accumulation of T cells on the compression side. Interestingly, it is reported that RANKL-positive activated T cells increase in mice transplanted with CD4 positive T cells.[15] Transplantation of T cells also increases the number of TNF-α and interferon-γ (INF-γ) positive cells on the compression side, indicating that T cells are one of the sources of inflammatory cytokines. Furthermore, Wald et al. [32] show that γδT cells, which are innate-like lymphocytes, contribute to the acceleration of OTM. This is demonstrated using Tcrd-GDL mice, allowing the conditional ablation of γδT cells under administration of diphtheria toxin, in which OTM is inhibited. They also report that a greater proportion of γδT cells reside in the gingiva, thereby proving that γδT cells contribute to OTM. γδT cells in PDL are mainly interleukin (IL)-17 producing Vγ6 positive γδT cells with an elevated expression of IL-17 during OTM. IL-17 has been reported to induce RANKL expression in PDL cells.[34] Taken together, these reports indicate that immune cells play a pivotal role in OTM through the RANKL-RANK pathway.
Osteoprotegerin (OPG) is a member of the TNF receptor family and plays a significant role in regulating osteogenesis by acting as a decoy receptor for RANKL, inhibiting RANKL-RANK signaling.[35] The regulation of bone remodeling depends on achieving a balance between OPG production and RANKL-RANK binding. The RANKL/OPG ratio is a determining factor in the formation of osteoclasts. In OPG-KO mice, osteopenia develops due to enhanced osteoclastogenesis.[36] Conversely, mice with OPG overexpression show a notable suppression of bone resorption, resulting in severe osteopetrosis.[35] The main source of OPG production in bone tissue is osteoblasts.[37] Clinically, OPG concentration in gingival crevicular fluid (GCF) significantly decreases after orthodontic force application.[38] In the compression side of OTM, bone resorption is facilitated by an up-regulation of RANKL and a down-regulation of OPG.[38,39] Local injection of OPG-Fc results in decreased OTM due to the inhibition of osteoclastogenesis.[40,41] From these findings, OPG is a decoy receptor against RANKL, and is involved in bone remodeling through the RANKL/RANK/OPG system.
SOST is a negative regulator of bone formation, which is encoded by the Sost gene and is primarily expressed by mature osteocytes. SOST binds to lipoprotein related peptide (LRP)5, LRP6, and frizzled receptors. It antagonizes osteoblast differentiation via inhibiting the Wnt/β-catenin signaling pathway. Deficiency in SOST gene results in high bone mass genetic disorders such as sclerosteosis.[42] Osteocytes translate mechanical loading into SOST production. For example, SOST expression is increased in unloaded sites in a tail suspension experiment.[43] In periodontal tissues, osteocytes in the alveolar bone express SOST, as revealed by Sost-LacZ mice.[44] During OTM, SOST is significantly increased on the compression side of the alveolar bone. One study postulates that when orthodontic force is initiated, bone cells of the compression side are unloaded, thereby increasing SOST expression.[45] By injecting SOST protein locally at the compression side of the alveolar bone, osteoclastogenesis is promoted in association with accelerated OTM.[46] It is also reported that osteoclastic activities and RANKL expression are reduced on the compression side in SOST-KO mice, resulting in a slower OTM rate. This indicates that osteoclastic activity and RANKL expression are decreased due to the lack of SOST.[47] SOST affects not only osteoclastogenesis but also osteogenesis. It is postulated that mesenchymal stem cells reside in the PDL and give rise to PDL cells and osteoblasts in the alveolar bone.[48] Gli1-positive cells in PDL include a population of mesenchymal stem cells termed PDL stem cells (PDLSCs). SOST suppresses PDLSCs activities by inhibiting the Wnt/β-catenin signaling pathway.[44] As a result, osteogenic capacity by PDLSCs is decreased, creating space for tooth movement on the compression side. Therefore, SOST is an important cytokine that can potentially accelerate OTM.
One aspect of orthodontic treatment is that it induces an aseptic inflammatory condition. OTM has been reported to increase inflammatory cytokines, such as TNF-α, IL-1, IL-6, and IFN-γ [49-51] (Fig. 1, Table 1). Since these cytokines are involved in osteoclastogenesis directly as well as indirectly through modulating inflammatory responses, it is important to understand how inflammatory cytokines regulate OTM.
TNF-α is expressed by activated macrophages, T and B lymphocytes, and natural killer cells.[52] Excessive activation of TNF-α signaling is associated with chronic inflammation. Mechanistically, TNF-α directly binds to receptors on the surface of osteoclasts and promotes osteoclastogenesis in a manner dependent on the RANKL/RANK axis.[53-55] Also, TNF-α stimulates RANK expression in osteoclast precursor cells.[56]
Administration of TNF-α inhibitor, etanercept, suppresses OTM.[33,57] Adoptive transfer experiments with T cells reveal that TNF-α positive cells accumulate on the compression side.[33] Similarity, M1 macrophages, known to produce inflammatory cytokines, increase the number of TNF-α positive cells, as shown by adoptive M1 macrophage transfer experiments.[57] These results indicate that TNF-α producing cells are primarily T cells and macrophages during OTM. Recently, an indirect mechanism of TNF-α in OTM has been reported. Ohori et al. [58] report that OTM is suppressed in TNF receptor (TNFR) 1 and TNFR2 double KO (dKO) mice. A decrease in SOST-positive osteocytes on the compression side is observed in TNFR dKO mice. This observation shows that TNF-α accelerates OTM by inducing SOST expression. In conclusion, TNF-α positively regulates OTM.
IL-1 regulates adaptive and innate immunity by binding to the IL-1 type 1 receptor (IL-1R). IL-1 is synthesized primarily by monocytes but also by activated macrophages, granulocytes, and endothelial cells.[59,60] The 2 forms of IL-1, IL-1α, and IL-1β have similar biological activities because of their common receptors on target cells. In addition to the immune response, IL-1 also promotes osteoclastogenesis. In vitro experiments show that the IL-1 administration upregulates RANKL expression in osteoblasts and promotes osteoclastogenesis.[61,62] IL-1α KO, IL-1β KO, and IL1-α/β dKO mice exhibited an increase of bone mass associated with a decrease in the number of osteoclasts.[63] These observations clearly indicate that excessive IL-1 signaling under pathological conditions enhances bone resorption. IL-1β is expressed on the compression side in OTM.[64] Additionally, IL-1R inhibitors reduce OTM associated with the decrease of osteoclasts.[65]
IL-6 is a cytokine with a pleiotropic effect on hematopoiesis, inflammation, immune responses, and bone homeostasis.[66] IL-6 is produced by various types of cells including immune cells, endothelial cells, adipocytes, and PDL cells. IL-6 is upregulated under inflammatory conditions such as periodontitis, rheumatoid arthritis and OTM.[67-69] Tsukasaki et al. [70] show that PDL cells highly express Il6 mRNA during periodontitis by in situ hybridization, indicating that PDL cells may act as a source of IL-6 in OTM. IL-6 binds to IL-6R and gp130 on osteoblastic cells. It activates the signal transducer and activator of transcription 3 (STAT3) activated in the cytoplasm by Janus kinase 2 (JAK2), inducing RANKL expression.[71,72] In osteoblastic deletion of Stat3 by Col1a1-CreER mice, OTM is inhibited due to the reduction in osteoblasts associated with a decrease in the number of osteoclasts on the compression side.[73] In experiments with a co-culture system of osteoblasts and osteoclasts under mechanical stimulation, Stat3-deficient osteoblasts show a lower osteoclast induction ability. These results may suggest that mechanical stimulation by orthodontic treatment affects osteoclastogenesis by upregulating RANKL expression in osteoblasts via the IL-6-induced JAK2/STAT3 signaling pathway.
IFN-γ is a cytokine that is critical for innate and adaptive immunity against viral and some bacterial infection. IFN-γ induces major histocompatibility complex (MHC) class II on antigen-presenting cells and stimulates macrophages and dendritic cells to phagocytose and kill bacteria.[74] Dual roles of IFN-γ in osteoclastogenesis have been reported. In vitro experiments reveal that the presence of IFN-γ strongly suppresses osteoclastogenesis.[75] On the other hand, IFN-γ also activates CD4+ T cells to produce RANKL and TNF-α through enhanced MHC class II expression on antigen-presenting cells.[76] In OTM, IFN-γ positive cells are accumulated on the compression side.[33,77] As the number of IFN-γ positive cells are decreased in nude mice, T cells are one of the cells that produce IFN-γ during OTM.[33] Yan et al. [33] show no significant changes in OTM after blockage of IFN-γ. On the other hand, Kohara et al. [78] report that IFN-γ injection decreases OTM by reducing the osteoclast number on the compression side. These results support the notion that IFN-γ acts via positive and negative pathways during OTM.
Most widely used medications in orthodontics are acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for control of pain following mechanical force application to the tooth. The use of NSAIDs reduces PGE2 by inhibiting 2 cyclooxygenase enzymes. When orthodontic force is applied, arachidonic acid is released from the lipid bilayer due to disruption of the cells on the pressure side. PGE2 is a well-known inflammatory mediator produced from arachidonic acid by constitutively expressed cyclooxygenase (COX)-1 and cytokine-inducible COX-2. COX-1 is mostly synthesized in normal tissues, while COX-2 is induced in inflammatory site.[79] Clinically, elevated PGE2 in the GCF is observed in patients undergoing orthodontic treatment.[49] This phenomenon occurs due to the PGE2 production by osteocytes and PDL cells in response to orthodontic forces.[80,81] From the 1980s, some orthodontists advocated that PGE2 accelerates OTM, since PGE2 acts directly on osteoclastogenesis.[82] The actions of PGE2 in the target cells are mediated by 4 different G protein-coupled receptor subtypes which are EP1, EP2, EP3, and EP4. Among PGE2 receptor subtypes, EP4 has been shown to mainly mediate PGE2-induced RANKL expression in osteoblasts.[82,83] OTM is accelerated in mice injected with PGE2.[84] These findings indicate that PGE2 produced by orthodontic forces promotes OTM.
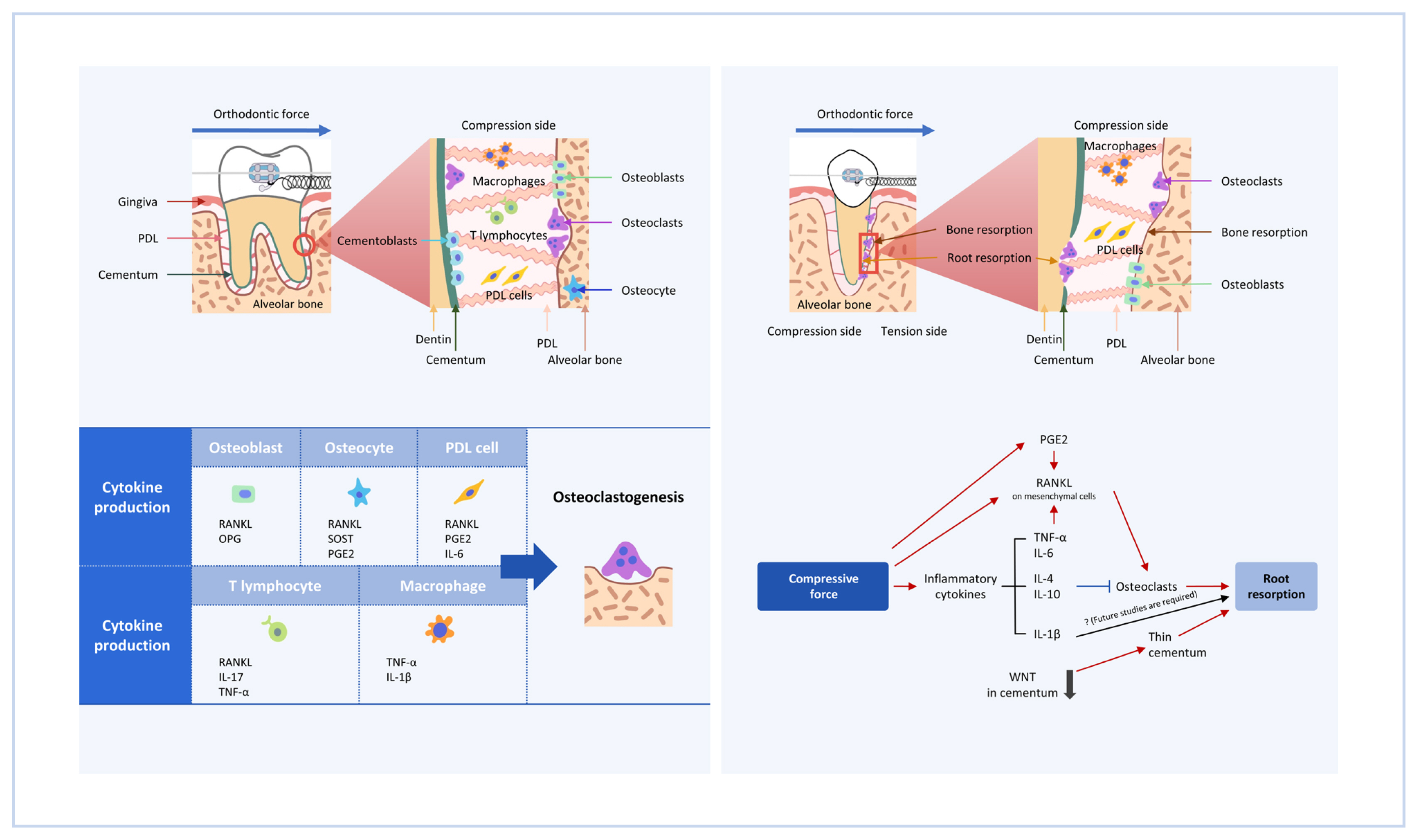
ERR occurs in various conditions, such as bacterial infection, trauma, and orthodontic treatment. Histologic studies reported over 90% of patients undergoing orthodontic treatment have some evidence of ERR.[85] The tooth root is protected from occlusal and orthodontic forces by the cementum. External dentin resorption would not occur unless full-thickness cemental resorption.[86] Proliferation and differentiation of cementoblasts are regulated by Wnt/β-catenin signaling. Loss of Wnt/β-catenin signaling in odontoblasts and osteoblasts by Ocn-cre induces a thinner cementum.[87] In other words, the reduction of canonical Wnt signaling negatively affects cementogenesis, resulting in a thinner cementum. This causes ERR without the application of orthodontic force, indicating cementoblasts are an important tissue that prevents ERR. In addition, ERR also occurs in the presence of cementum resorption by osteoclasts. Thus, pro-osteoclastic cytokines such as RANKL, TNF-α, and PGE2 facilitate ERR. M1 macrophages produce pro-inflammatory factors such as IL-6, TNF-α, and IL-1β, whereas M2 macrophages produce IL-4 and IL-10 which are involved in anti-inflammatory responses. He et al. [88] propose the M1/M2 ratio as one indicator of the progression of orthodontic induced ERR. Following the application of orthodontic force, an accumulation of CD68+iNOS+ M1 macrophages is observed at the ERR site. On the other hand, when orthodontic forces are removed, CD68+CD163+ M2-like macrophages increase. When the M1/M2 ratio is reduced by administration of IL-4, ERR is decreased. Fang et al. [89] also report that the inhibition of the CXCL12-CXCR4 axis with AMD 3100 suppresses the migration of M1 macrophages to the ERR sites and prevents orthodontic-induced ERR.
Several cytokines involved in RANKL expression induce ERR during OTM. Notch signaling pathway regulates cell growth, cell death, and differentiation programs via cell-cell communication. In the skeleton, 4 Notch receptors (Notch1 to −4) and 5 ligands (Delta1, −3, and −4 and Jagged [JAG]1 and −2) are expressed.[90] The JAG1-Notch2 signaling pathway induces RANKL expression on osteoblasts. Kikuta et al. [91] report that an increase in JAG1 and RANKL-positive cells around the ERR sites are observed during OTM. In vitro experiments indicate mechanical stimulation of human PDL (hPDL) cells increases JAG1 expression. The inhibition of Notch signaling by a selective γ-secretase inhibitor suppresses RANKL in hPDL cells.
Another cytokine that upregulates RANKL expression in periodontal tissues is parathyroid hormone (PTH)-related protein (PTHrP). PTHrP is a member of the PTH family secreted by defined skeletal cell types, including resting zone chondrocytes that include skeletal stem cells. During endochondral bone formation, PTHrP inhibits proliferating chondrocyte differentiation. In addition, PTHrP is involved in tooth eruption.[92,93] Dental follicle progenitor cells and cells around the root surface express PTHrP, and these cells contribute to tooth eruption via autocrine PTHrP-PTH1R signaling.[94] PTHrP induces RANKL expression in PDL cells.[95] RANKL on PDL cells has been reported to be involved in root resorption in deciduous teeth, thus PTHrP may be involved in ERR.[96]
Cytokines that promote osteoclastogenesis cause ERR, whereas the effect of IL-1β on OTM is controversial. Clinically, polymorphism at IL-1β genes which reduces the IL-1β cytokine production have higher risks to experience ERR.[97] P2X purinergic receptor 7 (P2X7) is an adenosine triphosphate (ATP)-gated ionotropic channel. It can be activated (opened) after binding to extracellular ATP, a danger signal from cells under mechanical stimuli. Opening the channel causes the accumulation of intracellular calcium and releases IL-1β. Viecilli et al. [98] reported that advanced ERR was observed in P2X7 KO mice during OTM. Similarly, OTM in IL-1β KO mice showed progression of ERR compared to wild-type mice.[99] On the other hand, IL-1β was originally discovered as a cytokine that induces bone degradation, and the positive effects on osteoclastogenesis are well established.[61-63,100] Furthermore, IL-1β and compressive forces lead to a significant induction of RANKL expression in primary human cementoblasts, indicating that the IL-1β production leads to ERR during OTM.[101] Therefore, future studies are required to elucidate the detailed molecular mechanisms by which IL-1β affects ERR.
As mentioned earlier, RANKL-positive cells promote ERR. RANKL is primarily produced as a membrane protein. Some membrane-bound RANKL is then shed by matrix metalloproteinases (MMPs) such as MMP13 and ADAM10 to form soluble RANKL.[102] Previous studies have reported that membrane-bound RANKL is a more potent inducer of osteoclastogenesis.[102,103] Soluble RANKL doesn’t contribute to osteoclastogenesis in young mice and OVX induced bone loss.[104,105] However, it is unclear whether soluble RANKL contributes to ERR. If soluble RANKL is not involved in ERR, osteoclasts that cause root resorption receive RANKL signaling through cell-cell contact around root resorption sites. This may establish a new treatment approach that suppresses ERR without affecting OTM by selectively inhibiting membrane-bound RANKL around root resorption areas.
In conclusion, cytokines that activate osteoclastogenesis, except IL-1β promote ERR (Fig. 2).
During OTM, bone formation by osteoblasts and bone resorption by osteoclasts are tightly regulated. In addition, recent studies implicate the importance of additional cell types, including osteocytes, immune cells and PDL cells for osteoclastogenesis. Complex signaling mediated by these cells causes osteoclastogenesis, making it difficult to comprehensively map cell-to-cell signaling networks. With the development of genetic engineering technology, it has become easier to analyze the function of specific cells for the purpose of elucidating the molecular mechanisms underlying OTM and ERR. This knowledge is expected to be clinically applicable to orthodontic treatment in the future. IL-1β acts positively on OTM, but its role in orthodontic-induced ERR is not fully understood. If IL-1β is proven to promote OTM without causing ERR, it would be one of the potential therapeutic targets.
Loss of Wnt/β-catenin signaling causes ERR under physiological conditions. Additionally, other genes involved in ERR have been reported.[106,107] However, only a limited number of studies have analyzed the function of these genes during OTM. Elucidating how these genes are involved in OTM is expected to pave the way for new orthodontic treatment modalities with fewer side effects.
DECLARATIONS
Fig. 1
Schematic diagram of orthodontic tooth movement (OTM). OTM is induced by applying orthodontic force to a tooth. On the side of the alveolar bone upon which the tooth root is compressed against (“compression side”), osteoclasts are formed to resorb the alveolar bone, to create a space to which the tooth root moves. Cytokines produced by several cell types, including osteoblasts, osteocytes, periodontal ligament (PDL) cells, lymphocytes and macrophages play roles in inducing osteoclastogenesis. RANKL, receptor activator of nuclear factor-κB ligand; OPG, osteoprotegerin; SOST, sclerostin; PGE2, prostaglandin E2; IL, interleukin; TNF, tumor necrosis factor.

Fig. 2
Schematic diagram of orthodontically induced external root resorption (ERR). Excessive orthodontic forces can induce a pathological condition termed orthodontically induced ERR, which is characterized by the resorption of the tooth root in addition to the alveolar bone. Cytokines that are involved in normal orthodontic tooth movement are also involved with tooth root resorption. PDL, periodontal ligament; PGE2, prostaglandin E2; RANKL, receptor activator of nuclear factor-κB ligand; TNF, tumor necrosis factor; IL, interleukin.
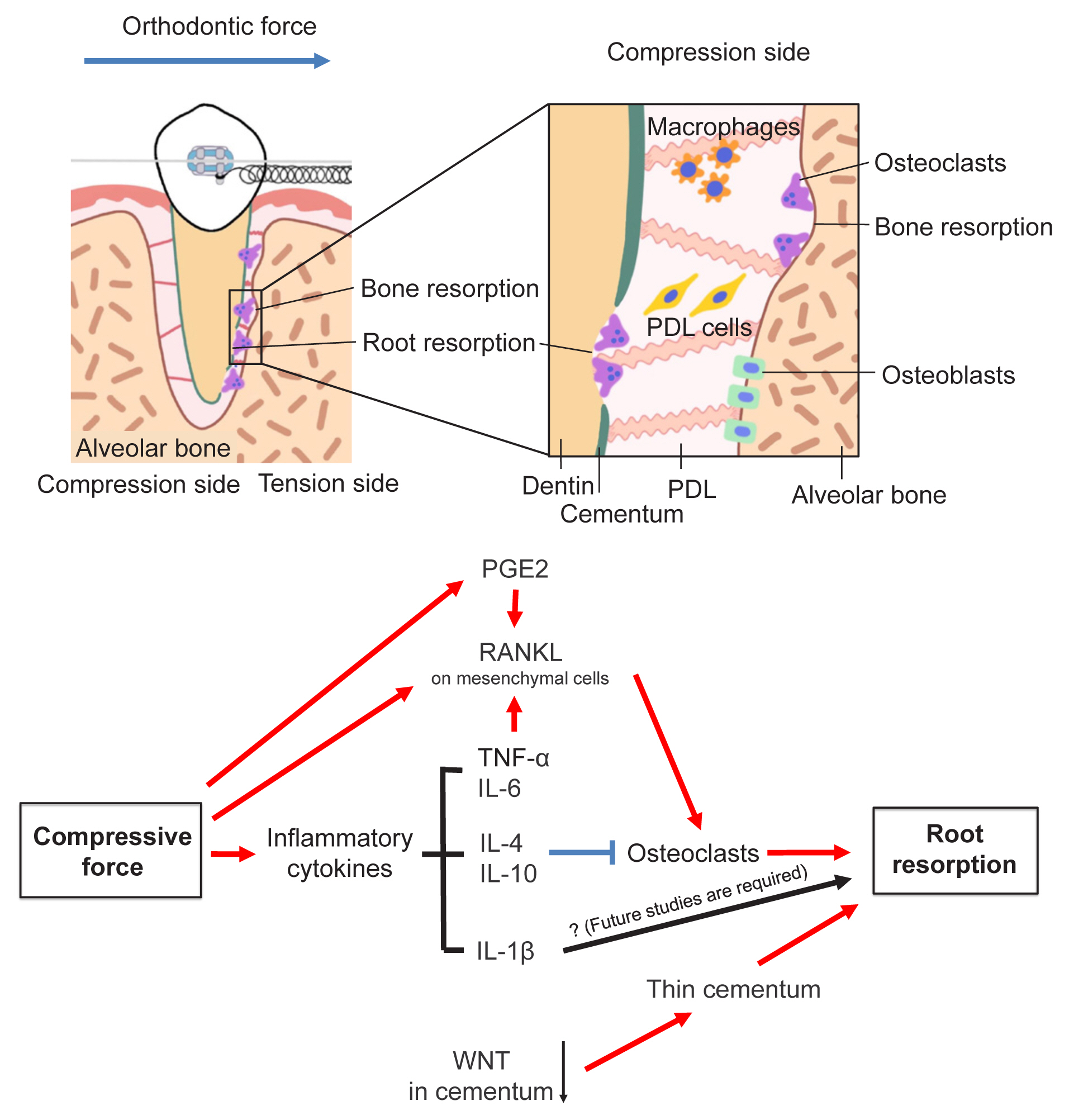
Table 1
Cytokine-producing cells that induce osteoclastogenesis during orthodontic tooth movement
| Cells | Cytokine | Mouse | Cell line | Reference |
|---|---|---|---|---|
| Osteoblast | RANKL | Col1a1-creER; Tnfsf11 cKO | Yang et al. (2018) [19] | |
|
|
||||
| PDL cells | RANKL | Col1a1-creER; Tnfsf11 cKO | Ogasawara et al. (2004) [17], Yang et al. (2018) [19], Miyazaki et al. (2021) [16] | |
| PGE2 | Human PDL fibroblasts | Ullrich et al. (2019) [80] | ||
|
|
||||
| Osteocytes | RANKL | Dmp1-cre; Tnfsf11 cKO | Shoji-Matsunaga et al. (2017) [14] | |
| Sclerostin | Sost −/− KO | MLO-Y4 cells | Shu et al. (2017) [47], Men et al. (2020) [44] | |
| PGE2 | MLO-Y4 cells | Kamel et al. (2010) [81] | ||
|
|
||||
| T cells | TNF-α, IFN-γ | Nude mice | Yan et al. (2015) [33] | |
| RANKL | Wu et al. (2020) [15] | |||
|
|
||||
| γδT cells | IL-17 | Tcrd-GDL mice | Wald et al. (2021) [32] | |
|
|
||||
| Macrophages | TNF-α | He et al. (2015) [57] | ||
PDL, periodontal ligament; RANKL, receptor activator of nuclear factor-κB ligand; PGE2, prostaglandin E2; TNF, tumor necrosis factor; IFN, interferon; IL-17, interleukin-17; Tnfsf11, tumor necrosis factor ligand superfamily member 11; cKO, conditional knockout; Dmp1, dentin matrix protein 1; Sost, sclerostin; KO, knockout; Tcrd, T-cell receptor delta chain; GDL, γδ-low; MLO-Y4, murine long bone osteocyte-Y4.
REFERENCES
1. Nagata M, English JD, Ono N, et al. Diverse stem cells for periodontal tissue formation and regeneration. Genesis 2022;60:e23495.
https://doi.org/10.1002/dvg.23495.



2. McCulloch CA, Lekic P, McKee MD. Role of physical forces in regulating the form and function of the periodontal ligament. Periodontol 2000 2000;24:56-72.
https://doi.org/10.1034/j.1600-0757.2000.2240104.x.


3. Yamaguchi M. RANK/RANKL/OPG during orthodontic tooth movement. Orthod Craniofac Res 2009;12:113-9.
https://doi.org/10.1111/j.1601-6343.2009.01444.x.


4. Huja SS, Fernandez SA, Hill KJ, et al. Remodeling dynamics in the alveolar process in skeletally mature dogs. Anat Rec A Discov Mol Cell Evol Biol 2006;288:1243-9.
https://doi.org/10.1002/ar.a.20396.



5. Son C, Choi MS, Park JC. Different responsiveness of alveolar bone and long bone to epithelial-mesenchymal interaction-related factor. JBMR Plus 2020;4:e10382.
https://doi.org/10.1002/jbm4.10382.



6. Chai Y, Jiang X, Ito Y, et al. Fate of the mammalian cranial neural crest during tooth and mandibular morphogenesis. Development 2000;127:1671-9.
https://doi.org/10.1242/dev.127.8.1671.


7. Alghamdi B, Jeon HH, Ni J, et al. Osteoimmunology in periodontitis and orthodontic tooth movement. Curr Osteoporos Rep 2023;21:128-46.
https://doi.org/10.1007/s11914-023-00774-x.


8. Suda T, Takahashi N, Udagawa N, et al. Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev 1999;20:345-57.
https://doi.org/10.1210/edrv.20.3.0367.


9. Kong YY, Yoshida H, Sarosi I, et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature 1999;397:315-23.
https://doi.org/10.1038/16852.


10. Yamaguchi M, Mishima H. The role of RANKL and involvement of cementum in orthodontic root resorption. Appl Sci (Basel) 2021;11:7244.
https://doi.org/10.3390/app11167244.

11. Yamaguchi M, Fukasawa S. Is inflammation a friend or foe for orthodontic treatment?: inflammation in orthodontically induced inflammatory root resorption and accelerating tooth movement. Int J Mol Sci 2021;22:2388.
https://doi.org/10.3390/ijms22052388.



12. Takayanagi H, Kim S, Koga T, et al. Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev Cell 2002;3:889-901.
https://doi.org/10.1016/s1534-5807(02)00369-6.


13. Pettit AR, Ji H, von Stechow D, et al. TRANCE/RANKL knockout mice are protected from bone erosion in a serum transfer model of arthritis. Am J Pathol 2001;159:1689-99.
https://doi.org/10.1016/s0002-9440(10)63016-7.



14. Shoji-Matsunaga A, Ono T, Hayashi M, et al. Osteocyte regulation of orthodontic force-mediated tooth movement via RANKL expression. Sci Rep 2017;7:8753.
https://doi.org/10.1038/s41598-017-09326-7.



15. Wu L, Su Y, Lin F, et al. MicroRNA-21 promotes orthodontic tooth movement by modulating the RANKL/OPG balance in T cells. Oral Dis 2020;26:370-80.
https://doi.org/10.1111/odi.13239.


16. Miyazaki T, Kurimoto R, Chiba T, et al. Mkx regulates the orthodontic tooth movement via osteoclast induction. J Bone Miner Metab 2021;39:780-6.
https://doi.org/10.1007/s00774-021-01233-2.


17. Ogasawara T, Yoshimine Y, Kiyoshima T, et al. In situ expression of RANKL, RANK, osteoprotegerin and cytokines in osteoclasts of rat periodontal tissue. J Periodontal Res 2004;39:42-9.
https://doi.org/10.1111/j.1600-0765.2004.00699.x.


18. Huang LH, Shotwell JL, Wang HL. Dental implants for orthodontic anchorage. Am J Orthod Dentofacial Orthop 2005;127:713-22.
https://doi.org/10.1016/j.ajodo.2004.02.019.

19. Yang CY, Jeon HH, Alshabab A, et al. RANKL deletion in periodontal ligament and bone lining cells blocks orthodontic tooth movement. Int J Oral Sci 2018;10:3.
https://doi.org/10.1038/s41368-017-0004-8.



20. Koda N, Sato T, Shinohara M, et al. The transcription factor mohawk homeobox regulates homeostasis of the periodontal ligament. Development 2017;144:313-20.
https://doi.org/10.1242/dev.135798.



21. Rangiani A, Jing Y, Ren Y, et al. Critical roles of periostin in the process of orthodontic tooth movement. Eur J Orthod 2016;38:373-8.
https://doi.org/10.1093/ejo/cjv071.



22. Nakashima T, Hayashi M, Fukunaga T, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med 2011;17:1231-4.
https://doi.org/10.1038/nm.2452.


23. Xiong J, Onal M, Jilka RL, et al. Matrix-embedded cells control osteoclast formation. Nat Med 2011;17:1235-41.
https://doi.org/10.1038/nm.2448.



24. Bonewald LF. The amazing osteocyte. J Bone Miner Res 2011;26:229-38.
https://doi.org/10.1002/jbmr.320.



25. Robling AG, Bonewald LF. The osteocyte: new insights. Annu Rev Physiol 2020;82:485-506.
https://doi.org/10.1146/annurev-physiol-021119-034332.



26. Matsumoto T, Iimura T, Ogura K, et al. The role of osteocytes in bone resorption during orthodontic tooth movement. J Dent Res 2013;92:340-5.
https://doi.org/10.1177/0022034513476037.


27. Xiong J, Piemontese M, Onal M, et al. Osteocytes, not osteoblasts or lining cells, are the main source of the RANKL required for osteoclast formation in remodeling bone. PLoS One 2015;10:e0138189.
https://doi.org/10.1371/journal.pone.0138189.



28. Zhang J, Link DC. Targeting of mesenchymal stromal cells by cre-recombinase transgenes commonly used to target osteoblast lineage cells. J Bone Miner Res 2016;31:2001-7.
https://doi.org/10.1002/jbmr.2877.

29. Cawley KM, Bustamante-Gomez NC, Guha AG, et al. Local production of osteoprotegerin by osteoblasts suppresses bone resorption. Cell Rep 2020;32:108052.
https://doi.org/10.1016/j.celrep.2020.108052.



30. Kacprzak A, Strzecki A. Methods of accelerating orthodontic tooth movement: a review of contemporary literature. Dent Med Probl 2018;55:197-206.
https://doi.org/10.17219/dmp/90989.


31. Wang Y, Zhang H, Sun W, et al. Macrophages mediate corticotomy-accelerated orthodontic tooth movement. Sci Rep 2018;8:16788.
https://doi.org/10.1038/s41598-018-34907-5.



32. Wald S, Leibowitz A, Aizenbud Y, et al. γδT cells are essential for orthodontic tooth movement. J Dent Res 2021;100:731-8.
https://doi.org/10.1177/0022034520984774.


33. Yan Y, Liu F, Kou X, et al. T cells are required for orthodontic tooth movement. J Dent Res 2015;94:1463-70.
https://doi.org/10.1177/0022034515595003.


34. Lin D, Li L, Sun Y, et al. IL-17 regulates the expressions of RANKL and OPG in human periodontal ligament cells via TRAF6/TBK1-JNK/NF-κB pathways. Immunology 2014;144:472-85.
https://doi.org/10.1111/imm.12395.



35. Simonet WS, Lacey DL, Dunstan CR, et al. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 1997;89:309-19.
https://doi.org/10.1016/s0092-8674(00)80209-3.


36. Bucay N, Sarosi I, Dunstan CR, et al. Osteoprotegerin-deficient mice develop early onset osteoporosis and arterial calcification. Genes Dev 1998;12:1260-8.
https://doi.org/10.1101/gad.12.9.1260.



37. Tsukasaki M, Asano T, Muro R, et al. OPG production matters where it happened. Cell Rep 2020;32:108124.
https://doi.org/10.1016/j.celrep.2020.108124.


38. Castroflorio T, Gamerro EF, Caviglia GP, et al. Biochemical markers of bone metabolism during early orthodontic tooth movement with aligners. Angle Orthod 2017;87:74-81.
https://doi.org/10.2319/022416-159.1.



39. Garlet TP, Coelho U, Silva JS, et al. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci 2007;115:355-62.
https://doi.org/10.1111/j.1600-0722.2007.00469.x.


40. Baxter SJ, Sydorak I, Ma PX, et al. Impact of pharmacologic inhibition of tooth movement on periodontal and tooth root tissues during orthodontic force application. Orthod Craniofac Res 2020;23:35-43.
https://doi.org/10.1111/ocr.12350.


41. Dunn MD, Park CH, Kostenuik PJ, et al. Local delivery of osteoprotegerin inhibits mechanically mediated bone modeling in orthodontic tooth movement. Bone 2007;41:446-55.
https://doi.org/10.1016/j.bone.2007.04.194.



42. Rauch F, Adachi R. Sclerostin: more than a bone formation brake. Sci Transl Med 2016;8:330fs7.
https://doi.org/10.1126/scitranslmed.aaf4628.


43. Robling AG, Niziolek PJ, Baldridge LA, et al. Mechanical stimulation of bone in vivo reduces osteocyte expression of Sost/sclerostin. J Biol Chem 2008;283:5866-75.
https://doi.org/10.1074/jbc.M705092200.


44. Men Y, Wang Y, Yi Y, et al. Gli1+ periodontium stem cells are regulated by osteocytes and occlusal force. Dev Cell 2020;54:639-54e6.
https://doi.org/10.1016/j.devcel.2020.06.006.


45. Nishiyama Y, Matsumoto T, Lee JW, et al. Changes in the spatial distribution of sclerostin in the osteocytic lacuno-canalicular system in alveolar bone due to orthodontic forces, as detected on multimodal confocal fluorescence imaging analyses. Arch Oral Biol 2015;60:45-54.
https://doi.org/10.1016/j.archoralbio.2014.08.013.


46. Lu W, Zhang X, Firth F, et al. Sclerostin injection enhances orthodontic tooth movement in rats. Arch Oral Biol 2019;99:43-50.
https://doi.org/10.1016/j.archoralbio.2018.12.011.


47. Shu R, Bai D, Sheu T, et al. Sclerostin promotes bone remodeling in the process of tooth movement. PLoS One 2017;12:e0167312.
https://doi.org/10.1371/journal.pone.0167312.



48. Nagata M, Ono N, Ono W. Mesenchymal progenitor regulation of tooth eruption: a view from PTHrP. J Dent Res 2020;99:133-42.
https://doi.org/10.1177/0022034519882692.



49. Ren Y, Vissink A. Cytokines in crevicular fluid and orthodontic tooth movement. Eur J Oral Sci 2008;116:89-97.
https://doi.org/10.1111/j.1600-0722.2007.00511.x.


50. Nunes L, Quintanilha L, Perinetti G, et al. Effect of orthodontic force on expression levels of ten cytokines in gingival crevicular fluid. Arch Oral Biol 2017;76:70-5.
https://doi.org/10.1016/j.archoralbio.2017.01.016.


51. Lowney JJ, Norton LA, Shafer DM, et al. Orthodontic forces increase tumor necrosis factor alpha in the human gingival sulcus. Am J Orthod Dentofacial Orthop 1995;108:519-24.
https://doi.org/10.1016/s0889-5406(95)70052-8.


52. Jang DI, Lee AH, Shin HY, et al. The role of tumor necrosis factor alpha (TNF-α) in autoimmune disease and current TNF-α inhibitors in therapeutics. Int J Mol Sci 2021;22:2719.
https://doi.org/10.3390/ijms22052719.



53. Lam J, Takeshita S, Barker JE, et al. TNF-alpha induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest 2000;106:1481-8.
https://doi.org/10.1172/jci11176.



54. Tanaka S. RANKL-independent osteoclastogenesis: a long-standing controversy. J Bone Miner Res 2017;32:431-3.
https://doi.org/10.1002/jbmr.3092.


55. Tsukasaki M, Hamada K, Okamoto K, et al. LOX fails to substitute for RANKL in osteoclastogenesis. J Bone Miner Res 2017;32:434-9.
https://doi.org/10.1002/jbmr.2990.


56. Kitaura H, Sands MS, Aya K, et al. Marrow stromal cells and osteoclast precursors differentially contribute to TNF-alpha-induced osteoclastogenesis in vivo. J Immunol 2004;173:4838-46.
https://doi.org/10.4049/jimmunol.173.8.4838.


57. He D, Kou X, Yang R, et al. M1-like macrophage polarization promotes orthodontic tooth movement. J Dent Res 2015;94:1286-94.
https://doi.org/10.1177/0022034515589714.


58. Ohori F, Kitaura H, Marahleh A, et al. Effect of TNF-α-induced sclerostin on osteocytes during orthodontic tooth movement. J Immunol Res 2019;2019:9716758.
https://doi.org/10.1155/2019/9716758.



60. Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev 2018;281:8-27.
https://doi.org/10.1111/imr.12621.



61. Wei S, Kitaura H, Zhou P, et al. IL-1 mediates TNF-induced osteoclastogenesis. J Clin Invest 2005;115:282-90.
https://doi.org/10.1172/jci23394.



62. Hofbauer LC, Lacey DL, Dunstan CR, et al. Interleukin-1beta and tumor necrosis factor-alpha, but not interleukin-6, stimulate osteoprotegerin ligand gene expression in human osteoblastic cells. Bone 1999;25:255-9.
https://doi.org/10.1016/s8756-3282(99)00162-3.


63. Lee YM, Fujikado N, Manaka H, et al. IL-1 plays an important role in the bone metabolism under physiological conditions. Int Immunol 2010;22:805-16.
https://doi.org/10.1093/intimm/dxq431.


64. Davidovitch Z, Nicolay OF, Ngan PW, et al. Neurotransmitters, cytokines, and the control of alveolar bone remodeling in orthodontics. Dent Clin North Am 1988;32:411-35.

65. Salla JT, Taddei SR, Queiroz-Junior CM, et al. The effect of IL-1 receptor antagonist on orthodontic tooth movement in mice. Arch Oral Biol 2012;57:519-24.
https://doi.org/10.1016/j.archoralbio.2011.09.018.


66. Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 2014;6:a016295.
https://doi.org/10.1101/cshperspect.a016295.



67. Jayaprakash PK, Basavanna JM, Grewal H, et al. Elevated levels of Interleukin (IL)-1β, IL-6, tumor necrosis factor-α, epidermal growth factor, and β2-microglobulin levels in gingival crevicular fluid during human orthodontic tooth movement (OTM). J Family Med Prim Care 2019;8:1602-6.
https://doi.org/10.4103/jfmpc.jfmpc_204_19.



68. Tsukasaki M. RANKL and osteoimmunology in periodontitis. J Bone Miner Metab 2021;39:82-90.
https://doi.org/10.1007/s00774-020-01165-3.


69. Okamoto K, Nakashima T, Shinohara M, et al. Osteoimmunology: the conceptual framework unifying the immune and skeletal systems. Physiol Rev 2017;97:1295-349.
https://doi.org/10.1152/physrev.00036.2016.


70. Tsukasaki M, Komatsu N, Nagashima K, et al. Host defense against oral microbiota by bone-damaging T cells. Nat Commun 2018;9:701.
https://doi.org/10.1038/s41467-018-03147-6.



71. Udagawa N, Takahashi N, Katagiri T, et al. Interleukin (IL)-6 induction of osteoclast differentiation depends on IL-6 receptors expressed on osteoblastic cells but not on osteoclast progenitors. J Exp Med 1995;182:1461-8.
https://doi.org/10.1084/jem.182.5.1461.



72. Palmqvist P, Persson E, Conaway HH, et al. IL-6, leukemia inhibitory factor, and oncostatin M stimulate bone resorption and regulate the expression of receptor activator of NF-kappa B ligand, osteoprotegerin, and receptor activator of NF-kappa B in mouse calvariae. J Immunol 2002;169:3353-62.
https://doi.org/10.4049/jimmunol.169.6.3353.


73. Gong X, Sun S, Yang Y, et al. Osteoblastic STAT3 is crucial for orthodontic force driving alveolar bone remodeling and tooth movement. J Bone Miner Res 2023;38:214-27.
https://doi.org/10.1002/jbmr.4744.


74. Ivashkiv LB. IFNγ: signalling, epigenetics and roles in immunity, metabolism, disease and cancer immunotherapy. Nat Rev Immunol 2018;18:545-58.
https://doi.org/10.1038/s41577-018-0029-z.



75. Takayanagi H, Ogasawara K, Hida S, et al. T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-gamma. Nature 2000;408:600-5.
https://doi.org/10.1038/35046102.


76. Kato M. New insights into IFN-γ in rheumatoid arthritis: role in the era of JAK inhibitors. Immunol Med 2020;43:72-8.
https://doi.org/10.1080/25785826.2020.1751908.


77. Alhashimi N, Frithiof L, Brudvik P, et al. Orthodontic movement induces high numbers of cells expressing IFN-gamma at mRNA and protein levels. J Interferon Cytokine Res 2000;20:7-12.
https://doi.org/10.1089/107999000312685.


78. Kohara H, Kitaura H, Yoshimatsu M, et al. Inhibitory effect of interferon-γ on experimental tooth movement in mice. J Interferon Cytokine Res 2012;32:426-31.
https://doi.org/10.1089/jir.2011.0124.


79. FitzGerald GA. COX-2 and beyond: approaches to prostaglandin inhibition in human disease. Nat Rev Drug Discov 2003;2:879-90.
https://doi.org/10.1038/nrd1225.


80. Ullrich N, Schröder A, Jantsch J, et al. The role of mechanotransduction versus hypoxia during simulated orthodontic compressive strain-an in vitro study of human periodontal ligament fibroblasts. Int J Oral Sci 2019;11:33.
https://doi.org/10.1038/s41368-019-0066-x.



81. Kamel MA, Picconi JL, Lara-Castillo N, et al. Activation of β-catenin signaling in MLO-Y4 osteocytic cells versus 2T3 osteoblastic cells by fluid flow shear stress and PGE2: implications for the study of mechanosensation in bone. Bone 2010;47:872-81.
https://doi.org/10.1016/j.bone.2010.08.007.



82. Suzawa T, Miyaura C, Inada M, et al. The role of prostaglandin E receptor subtypes (EP1, EP2, EP3, and EP4) in bone resorption: an analysis using specific agonists for the respective EPs. Endocrinology 2000;141:1554-9.
https://doi.org/10.1210/endo.141.4.7405.


83. Tomita M, Li X, Okada Y, et al. Effects of selective prostaglandin EP4 receptor antagonist on osteoclast formation and bone resorption in vitro. Bone 2002;30:159-63.
https://doi.org/10.1016/s8756-3282(01)00688-3.


84. Leiker BJ, Nanda RS, Currier GF, et al. The effects of exogenous prostaglandins on orthodontic tooth movement in rats. Am J Orthod Dentofacial Orthop 1995;108:380-8.
https://doi.org/10.1016/s0889-5406(95)70035-8.


85. Weltman B, Vig KW, Fields HW, et al. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop 2010;137:462-76. discussion 12A https://doi.org/10.1016/j.ajodo.2009.06.021.


86. Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod 2002;72:175-9.
https://doi.org/10.1043/0003-3219(2002)072<0175:Oiirrp>2.0.Co;2.


87. Zhang R, Yang G, Wu X, et al. Disruption of Wnt/β-catenin signaling in odontoblasts and cementoblasts arrests tooth root development in postnatal mouse teeth. Int J Biol Sci 2013;9:228-36.
https://doi.org/10.7150/ijbs.5476.



88. He D, Kou X, Luo Q, et al. Enhanced M1/M2 macrophage ratio promotes orthodontic root resorption. J Dent Res 2015;94:129-39.
https://doi.org/10.1177/0022034514553817.


89. Fang XY, Zhan YX, Zhou XM, et al. CXCL12/CXCR4 mediates orthodontic root resorption via regulating the M1/M2 ratio. J Dent Res 2022;101:569-79.
https://doi.org/10.1177/00220345211050324.

90. Zhou B, Lin W, Long Y, et al. Notch signaling pathway: architecture, disease, and therapeutics. Signal Transduct Target Ther 2022;7:95.
https://doi.org/10.1038/s41392-022-00934-y.



91. Kikuta J, Yamaguchi M, Shimizu M, et al. Notch signaling induces root resorption via RANKL and IL-6 from hPDL cells. J Dent Res 2015;94:140-7.
https://doi.org/10.1177/0022034514555364.


92. Arai Y, English JD, Ono N, et al. Effects of antiresorptive medications on tooth root formation and tooth eruption in paediatric patients. Orthod Craniofac Res 2023;
https://doi.org/10.1111/ocr.12637.


93. Ono W, Sakagami N, Nishimori S, et al. Parathyroid hormone receptor signalling in osterix-expressing mesenchymal progenitors is essential for tooth root formation. Nat Commun 2016;7:11277.
https://doi.org/10.1038/ncomms11277.



94. Takahashi A, Nagata M, Gupta A, et al. Autocrine regulation of mesenchymal progenitor cell fates orchestrates tooth eruption. Proc Natl Acad Sci U S A 2019;116:575-80.
https://doi.org/10.1073/pnas.1810200115.



95. Fukushima H, Jimi E, Kajiya H, et al. Parathyroid-hormone-related protein induces expression of receptor activator of NF-{kappa}B ligand in human periodontal ligament cells via a cAMP/protein kinase A-independent pathway. J Dent Res 2005;84:329-34.
https://doi.org/10.1177/154405910508400407.


96. Fukushima H, Kajiya H, Takada K, et al. Expression and role of RANKL in periodontal ligament cells during physiological root-resorption in human deciduous teeth. Eur J Oral Sci 2003;111:346-52.
https://doi.org/10.1034/j.1600-0722.2003.00051.x.


97. Al-Qawasmi RA, Hartsfield JK Jr, Everett ET, et al. Genetic predisposition to external apical root resorption. Am J Orthod Dentofacial Orthop 2003;123:242-52.
https://doi.org/10.1067/mod.2003.42.


98. Viecilli RF, Katona TR, Chen J, et al. Orthodontic mechanotransduction and the role of the P2X7 receptor. Am J Orthod Dentofacial Orthop 2009;135:694e1-16.
https://doi.org/10.1016/j.ajodo.2008.10.018.


99. Al-Qawasmi RA, Hartsfield JK Jr, Everett ET, et al. Root resorption associated with orthodontic force in inbred mice: genetic contributions. Eur J Orthod 2006;28:13-9.
https://doi.org/10.1093/ejo/cji090.


100. Horton JE, Raisz LG, Simmons HA, et al. Bone resorbing activity in supernatant fluid from cultured human peripheral blood leukocytes. Science 1972;177:793-5.
https://doi.org/10.1126/science.177.4051.793.


101. Diercke K, Kohl A, Lux CJ, et al. IL-1β and compressive forces lead to a significant induction of RANKL-expression in primary human cementoblasts. J Orofac Orthop 2012;73:397-412.
https://doi.org/10.1007/s00056-012-0095-y.


102. Hikita A, Yana I, Wakeyama H, et al. Negative regulation of osteoclastogenesis by ectodomain shedding of receptor activator of NF-kappaB ligand. J Biol Chem 2006;281:36846-55.
https://doi.org/10.1074/jbc.M606656200.


103. Nakashima T, Kobayashi Y, Yamasaki S, et al. Protein expression and functional difference of membrane-bound and soluble receptor activator of NF-kappaB ligand: modulation of the expression by osteotropic factors and cytokines. Biochem Biophys Res Commun 2000;275:768-75.
https://doi.org/10.1006/bbrc.2000.3379.


104. Xiong J, Cawley K, Piemontese M, et al. Soluble RANKL contributes to osteoclast formation in adult mice but not ovariectomy-induced bone loss. Nat Commun 2018;9:2909.
https://doi.org/10.1038/s41467-018-05244-y.



105. Asano T, Okamoto K, Nakai Y, et al. Soluble RANKL is physiologically dispensable but accelerates tumour metastasis to bone. Nat Metab 2019;1:868-75.
https://doi.org/10.1038/s42255-019-0104-1.


106. Decker MG, Nottmeier C, Luther J, et al. Role of c-Fos in orthodontic tooth movement: an in vivo study using transgenic mice. Clin Oral Investig 2021;25:593-601.
https://doi.org/10.1007/s00784-020-03503-1.



107. Zhang X, Li Z, Zhao Z, et al. Runx1/miR-26a/Jagged1 signaling axis controls osteoclastogenesis and alleviates orthodontically induced inflammatory root resorption. Int Immunopharmacol 2021;100:107991.
https://doi.org/10.1016/j.intimp.2021.107991.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 2,139 View
- 76 Download
- ORCID iDs
-
Wanida Ono

https://orcid.org/0000-0002-0358-1897Noriaki Ono

https://orcid.org/0000-0002-3771-8230 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



