Effect Modification on Death by Age and Sex in Elderly Hip Fracture
Article information
Abstract
Background
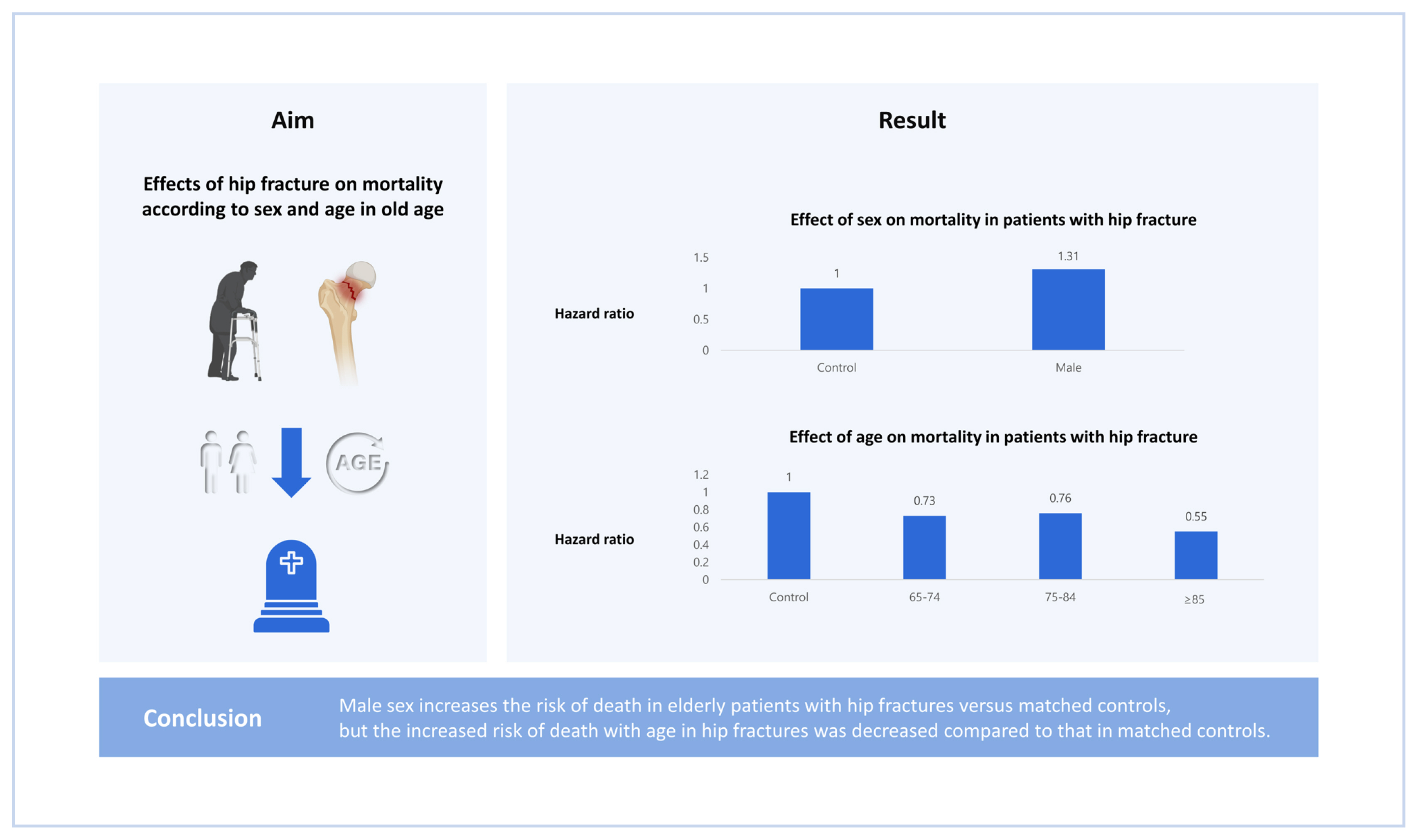
This study compared the effects of hip fractures on mortality according to sex and age in a nationwide cohort of elderly patients with hip fractures and controls.
Methods
Patients with hip fractures and matched controls were selected from the National Health Insurance Service-Senior cohort. Time-dependent propensity score matching was estimated from a Cox proportional hazards model with January 1, 2005, as the baseline and hip fracture as an event. Patients were matched by age and sex to participants at risk of developing a hip fracture at time zero. The effect size is presented as hazard ratio (HR) using a Cox proportional hazards model with a robust variance estimator that accounts for clustering within the matched pairs.
Results
Altogether, 14,283 patients with incident hip fractures and 28,566 matched controls were identified. The HR of male sex in hip fractures was 1.31 (95% confidence interval [CI], 1.22–1.40; Pinteraction<0.01). Moreover, the HR of age group in hip fractures was 0.73 (95% CI, 0.66–0.80; Pinteraction< 0.01) between the 65 to 74 and 75 to 84 years groups, 0.76 (95% CI, 0.71–0.81; Pinteraction< 0.01) between the 75 to 84 and ≥85 years groups, and 0.55 (95% CI, 0.50–0.61; Pinteraction< 0.01) between the 65 to 74 and ≥85 years groups.
Conclusions
Male sex increases the risk of death in elderly patients with hip fractures versus matched controls, but the increased risk of death with age in hip fractures was decreased compared to that in matched controls.
INTRODUCTION
In older age, hip fracture is well known as an injury that reduces the patient’s functional ability and has an economic impact on the patient’s family due to the high cost of treatment.[1,2] This is a socioeconomic problem in developed countries and management of osteoporosis is important to prevent hip fractures.[3,4] However, among the negative effects caused by hip fractures, one of the main things we notice is the increase in mortality after a fracture.[5] This is because these patients have a lot of comorbidities as well as old age.[5,6] Many studies have been conducted on factors that increase the risk of death in older patients with hip fractures.[7–10]
There have already been many reports of changes in mortality risk with age and sex in hip fracture patients.[11–20] Bliuc et al. [21] analyzed the mortality of men and women over 60 using a prospective cohort in Dubbo, Australia. They presented age- and sex-standardized mortality ratios (SMR) by comparing hip fracture patients to the overall population. Wang et al. [22] conducted a mortality analysis of hip fracture patients using the Taiwan National Health Insurance database. The risk of death was higher in older people, and the risk of death in men was higher than in women. However, these studies did not adjust the characteristics of demographic factors in the control group to reflect comorbidities in older patients with hip fractures, and only the sex or age is adjusted to present the risk ratio using an indirect standardized mortality rate. In addition, due to the statistical limitations of past studies, there was a lack of statistical verification of comparisons between risks increased by hip fracture according to age group.
Therefore, this study constructed a matched control group of hip fractures in Korea nationwide cohort using time-dependent propensity score matching and compared the effects of hip fracture on mortality according to sex and age group by comparing elderly patients with hip fractures to control groups similar to socioeconomic factors and demographic factors including their sex, age, as well as a comorbidity in a nationwide cohort.
METHODS
Hip fracture patients and their matched controls were selected from the National Health Insurance Service-Senior cohort (NHIS-Senior version 1) of South Korea. The NHIS established the National Health Information Database (NHID) a claims database for research purposes that stores all records of healthcare and long-term care services.[23,24] From the NHID, the NHIS constructed and provided researchers with the NHIS-Senior cohort, representative administrative data for health policy and medical research purposes. The NHIS published a detailed cohort profile in the literature.[24] The NHIS-Senior consists of 558,147 people selected by 10% simple random sampling method from a total of 5.5 million subjects aged 60 or over in 2002.[24] Under a compulsory social insurance system by the National Health Insurance Act, all subjects could be followed up until 2015, except for instances of death or emigration.[24,25] The NHIS maintains all personal information, demographics, and medical treatment data for the entire Korean population.[25,26] The key variables in the NHIS-Senior cohort include all inpatient and outpatient medical claims data such as codes for a treatment procedure, prescription, and diagnosis. The design and protocol of this study were approved by the Institutional Review Board (IRB) in our hospital (IRB no. EMC 2019-06-019).
1. Incident hip fracture cohort
The incident hip fracture cohort was constructed from the NHIS-Senior cohort as the base cohort. Considering previous studies, the inclusion criteria for the study sample were as follows [27–30]:
•First-time admission during the follow-up period (2002 to 2015) to an acute care hospital (index admission) with diagnostic codes of femoral neck fractures (International Classification of Diseases, Tenth Revision [ICD-10] S720) or intertrochanteric fracture (ICD-10 S721); and
•Patients underwent surgeries including internal fixation (open reduction of fractured extremity or closed pinning [femur]), hemiarthroplasty, or total arthroplasty (hip).
Some patients who met the inclusion criteria were excluded for the validity of the study design:
•Patients with hip fractures prior to January 1, 2005 were excluded to ensure a minimum 3-year hip fracture-free period.
•Patients under the Medical Aid program were excluded to eliminate the possibility of incomplete information.
The incidence date (time-zero) of hip fracture was defined as the date of admission to the acute care hospital that fulfilled the inclusion criteria. Incident hip fracture patients were enrolled to the incident hip fracture cohort at time-zero and followed up thereafter.
2. All-cause mortality
In the NHIS-Senior, each subject’s unique de-identified number was linked to vital statistics, including dates and causes of death, from the Korean National Statistical Office.[24] The dates of death from the mortality information were used to calculate the survival times.
3. Risk-set matching on propensity score
The time-dependent propensity score was first calculated, then risk-set matching was performed.[31,32] To adjust for confounding effects, the association between hip fracture and risk of death was examined through time-dependent propensity score matching.[32] Propensity scores were estimated from Cox’s proportional-hazards model with January 1, 2005 as the baseline and hip fracture as an event. All variables included in Table 1 were included as independent variables. All variables were identified from 3 years (2002–2004) before the baseline (January 1, 2005). Age and square of age were included as continuous variables; sex, household income level (decile), type of National Health Insurance, registered disability, residential district as fixed effect, Charlson Comorbidity Index (CCI), a number of hospital admissions, past medication history, and past medical history were categorical variables. Each subject’s comorbidities were assessed by diagnostic codes using the Quan ICD-10 coding algorithm of the CCI score.[33] Prescriptions of over 90 days for antihypertensive, antidiabetic, lipid-lowering, and anti-depressive agents were considered for patients who have taken corresponding medications.
The patient was matched to subjects at risk of developing a hip fracture with the same age and sex at time-zero was identified. Then, this method of risk-set matching was repeated sequentially for the next patient until the last hip fracture patient.[31,34,35] A 1:2 matching on the propensity score was then sequentially performed for each risk set using the nearest neighbor matching algorithm with a maximum caliber of 0.1 of the hazard components. To make the matching independent of future events, the matched control subjects could either be those who never developed or were yet to develop hip fractures. A hip fracture patient in the incident hip fracture cohort could, therefore, enter the study as a hip fracture patient or a matched control for the other hip fracture patient whose time-zero was prior to that patient.[36] Next, to yield non-overlapping samples from the risk set, the matched subjects were removed from the next risk sets. The same process continued and was repeated with the next risk set. The matching process stopped when there were no more treated patients in the risk set.
4. Statistical analyses
Using final matched cohorts, statistical tests for the association between incident hip fracture and death according to age and sex were performed with the statistical nature of the matched pair analysis taken into consideration. To assess covariate balance between treatment groups, baseline characteristics were compared with standardized differences (STD), where a difference of less than 0.1 (10%) is generally considered negligible.[37,38] The effect size was presented as hazard ratio (HR) using Cox’s proportional hazard model with a robust variance estimator that accounts for clustering within matched pairs.[37,38] Time-zero was set to the date of hip fracture for both hip fracture patients and their matched controls. Survival time was defined by days from the incidence date (time-zero) to the date of death or December 31, 2015, whichever comes first. Statistical analyses were conducted using SAS Enterprise Guide version 7.1 (SAS Institute Inc., Cary, NC, USA). All P values of less than 0.05 were considered statistically significant.
RESULTS
The final sample that met the inclusion criteria was 19,460 (January 1, 2002 to December 31, 2015). Among these patients, the occurrence of hip fracture during the first 3 years (2002–2004; 1,912 patients), and enrollees of the Medical Aid program (2,305 patients) were excluded following the exclusion criteria (Fig. 1). Nine hundred sixty hip fracture patients, whom at the time of risk-set matching had no fractures, entered into the study as control subjects. A total of 14,283 incident hip fracture patients and their 28,566 matched controls remained in the study. The mean follow-up time was 3.95±2.90 years, generating 169,380.37 person-years.
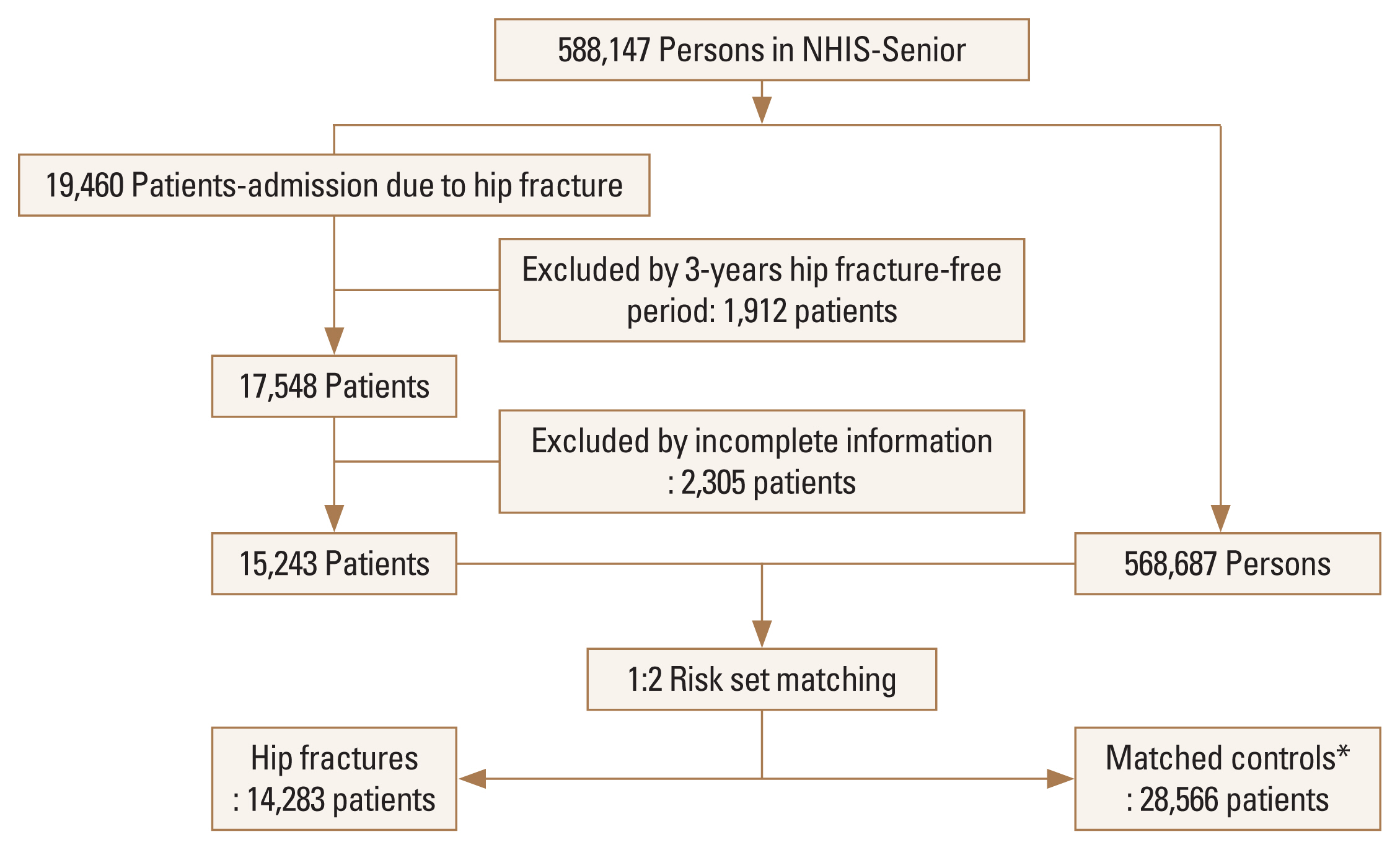
Flow chart of this study. *During risk-set matching, 960 hip fracture patients entered into the study as control subjects of another hip fracture patient. NHIS, National Health Insurance Service.
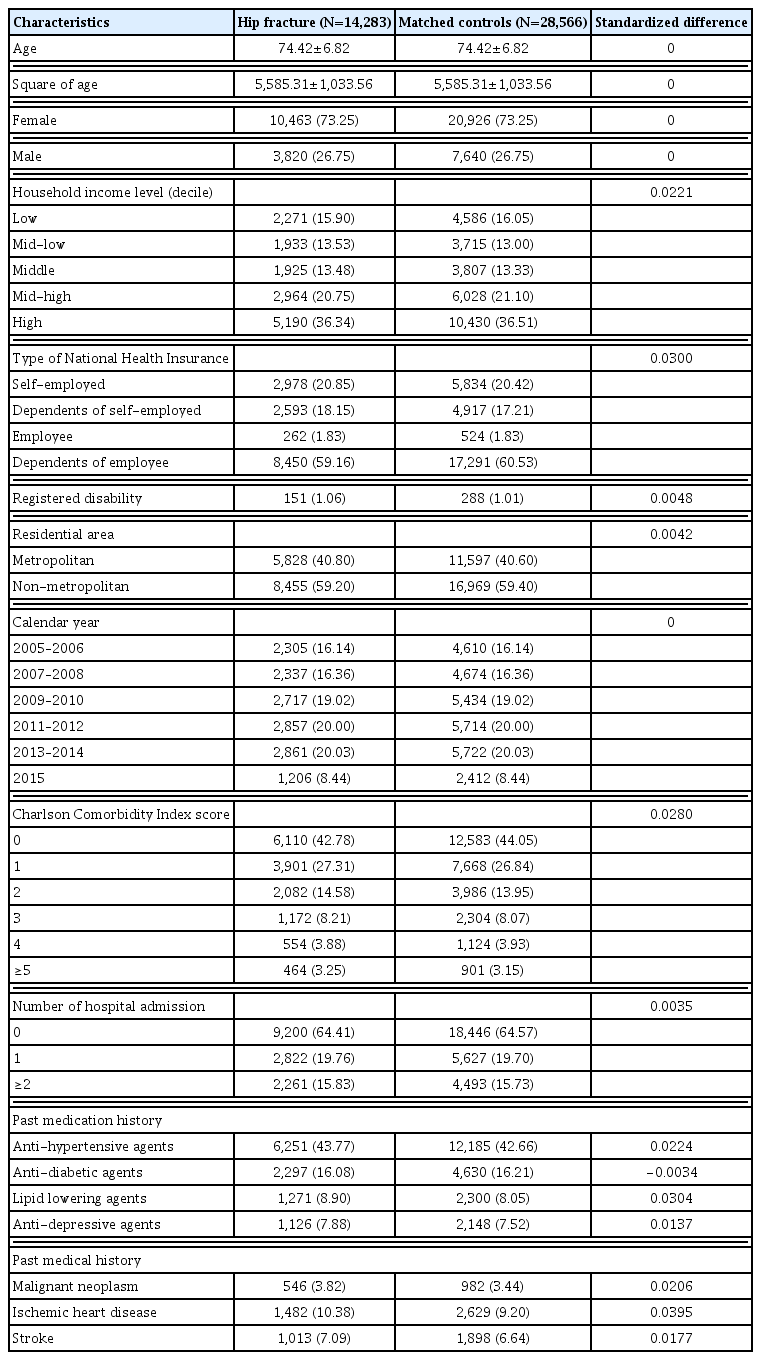
Table 1 shows the baseline characteristics of the matched cohorts. The mean age was 74.42 (standard deviation, ±6.82) years, and 73.25% were female. In both groups, the proportion of 65 to 74 group, 75 to 84 group, and ≥85 group was 19.83%, 51.19%, and 28.98%, respectively.
In the matched control group, the risk of death was 1.21 times (HR, 1.21; 95% confidence interval [CI], 1.15–1.27; P<0.01) higher for men than for women (Fig. 2). In hip fracture group, the risk of death was 1.58 times (HR, 1.58; 95% CI, 1.50–1.66; P<0.01) higher for men than for women. Thus, effect modification by a male in hip fracture group was 1.31 times (HR, 1.31; 95% CI, 1.22–1.40; Pinteraction<0.01).
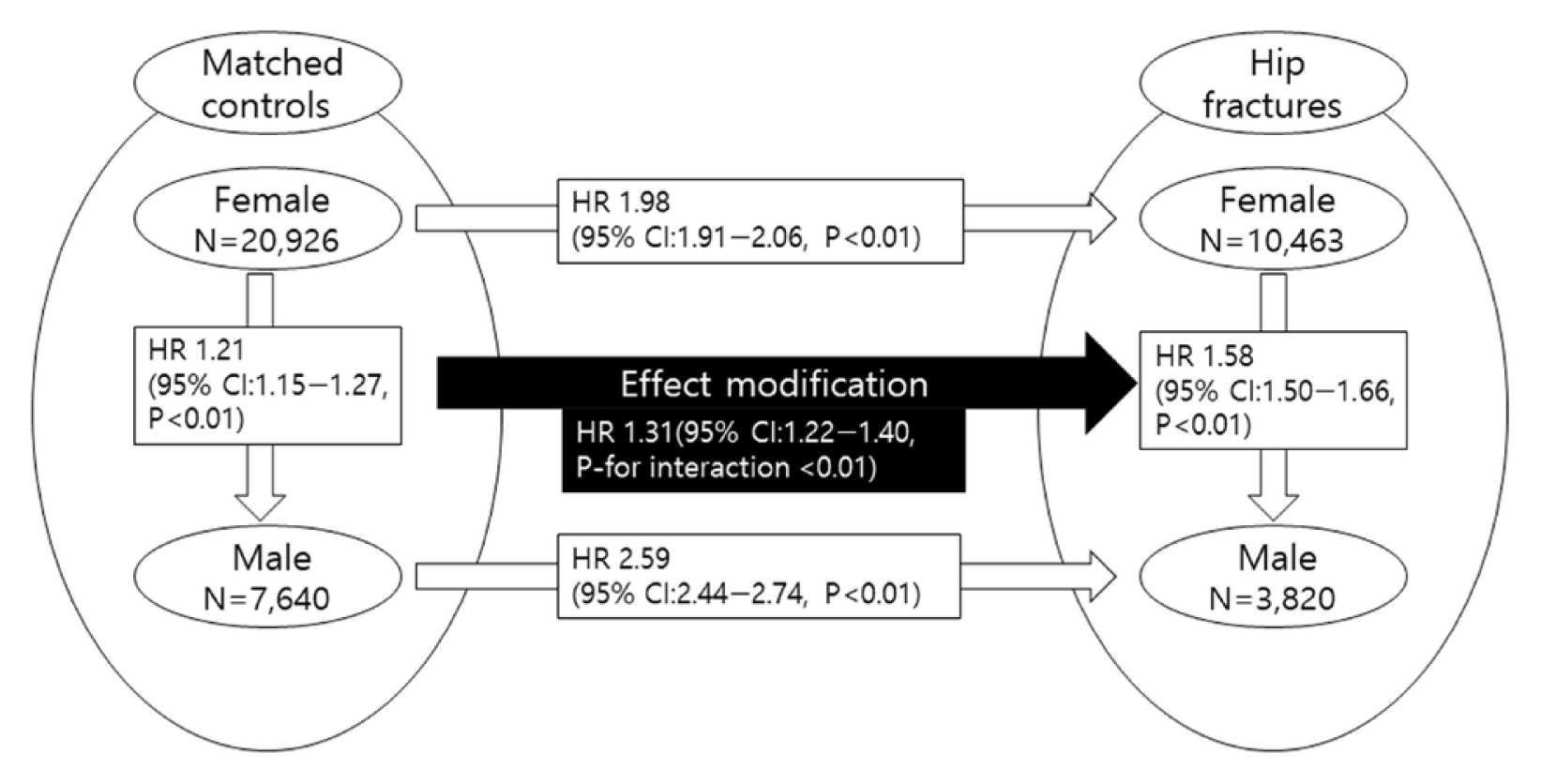
According to sex, comparison of risk of death between elderly hip fracture patients and their risk-set matched controls. HR, hazard ratio; CI, confidence interval.
Compared with the 65 to 74 group, the risk of death of the 75 to 84 group and ≥85 group was 2.36 times (HR, 2.36; 95% CI, 2.19–2.55; P<0.01) and 5.77 times (HR, 5.77; 95% CI, 5.35–6.22; P<0.01) higher in the matched control group, and 1.71 times (HR, 1.71; 95% CI, 1.60–1.84; P<0.01) and 3.17 times (HR, 3.17; 95% CI, 2.95–3.41; P<0.01) higher in the hip fracture group (Fig. 3). Compared with the 75 to 84 group, the risk of death of ≥85 group was 2.45 times (HR, 2.45; 95% CI, 2.33–2.56; P<0.01) higher in the matched control group, and 1.85 times (HR, 1.85; 95% CI, 1.76–1.95; P<0.01) higher in the hip fracture group. Thus, effect modification by age group in hip fracture group was 0.73 times (HR, 0.73; 95% CI, 0.66–0.80; Pinteraction<0.01) between 65 to 74 group and 75 to 84 group, 0.76 times (HR, 0.76; 95% CI, 0.71–0.81; Pinteraction<0.01) between 75 to 84 group and ≥85 group, and 0.55 times (HR, 0.55; 95% CI, 0.50–0.61; Pinteraction<0.01) between 65 to 74 group and ≥85 group.
DISCUSSION
The main findings of this study are as follows (1) Because the effect modification on death by male in hip fracture was 1.31 times, male sex more increased risk of death in hip fracture compared to the matched control group; (2) Older patients in hip fracture have more risk of death compared to younger patients. However, considering the increased risk of death by age in the matched control group, the increased risk of death in hip fracture by older age rather decreased.
In the general population, the risk of death increases with aging, and male have higher mortality rates than women in age 65 years over.[39] A decrease in immune competence due to aging is presumed to be one of the causes of the high mortality rate of hip fracture, and it is also explained that this change is greater in male than in female.[12,39] In addition, in hip fracture patients, male and older patients have more preoperative comorbidity and a higher postoperative complication rate.[12] However, when interpreting the results of death risk in patients with hip fractures, it is necessary to take into account the increase in the risk of death according to the age and sex of the general population.
Previously, studies that analyzed the effects of mortality by age and sex in older patients with hip fractures had some statistical analysis problems and errors in their interpretation. Haentjens et al. [12] compared the survival of the hip fracture group in a meta-analysis using prospective cohort studies with age- and sex-matched control groups and analyzed the risk of death for men and women in hip fracture. In this study, the risk of death increased by 8 times in men and 5 times in women within 3 months after surgery and approximately increased by 3 times within 15 years after injury. However, in our study, the increased risk of death from hip fracture was 1.98 times in women and 2.59 times in men. The significant difference in the risk of death between the 2 studies is that the cohort of the study has different aspects, but there are differences in variables used in matching with the control group. Yoon et al. [5] investigated the risk of death by sex in an analysis of mortality in hip fracture patients over 50 years old in a nationwide cohort and reported age and sex-adjusted SMR. Therefore, the risk of death in the hip fracture group may be overestimated because the comorbidities of hip fracture were not considered in these studies and only age and sex were used as adjusted variables. Our study analyzed the difference in mortality risk by sex in elderly patients with hip fractures using propensity score matching considering all demographic factors including underlying disease, socioeconomic factors, and hip fracture date. In addition, statistical analysis between risks of death proved that the risk of death by male sex in hip fracture patients was 1.31 times.
Bliuc et al. [21] used a prospective cohort from Dubbo, Australia, to analyze age-related mortality risk in hip fracture patients over 60. They also used age-adjusted SMR and analyzed the results compared to the general population. They reported that the risk of death for hip fracture patients aged 60 to 74 years was 2.43 times for men and 8.28 times for women, 2.24 times and 3.65 times for hip fracture patients over 75. Their results suggested that the risk of death for each age group in hip fracture patients was adjusted only by age group, and no statistical comparative analysis between the risks of death for each age group was performed. Yoon et al. [5] also reported age and sex-adjusted SMR of hip fracture. They reported that the highest SMR in each age group was observed at 50 to 59 years. However, the comparison of the presented SMR is a misinterpretation. Comparisons between SMR presented in each age group should be made through appropriate statistical analysis. Our study statistically demonstrated the effect of modification on the increase in mortality risk with increasing age of hip fracture group. In addition, it was found that the increase in mortality risk with age was smaller in patients with hip fractures compared to the increase in mortality risk with age in the general population. And we believe that this means that hip fracture has a significant effect on mortality to the extent that it reduces the effect of increased mortality with increasing age.
While the present study attempted to fill in the gaps in present literature, the study is limited to available information on the cohort. Variables such as the severity of hip fracture were thus not included in the model to calculate propensity score, which may result in residual confounding after propensity score matching. Disease codes of the inclusion criteria may also not represent the actual status of a patient’s disease, being a fundamental limitation of the insurance database. However, the incidence of hip fracture could be ascertained well because almost all hospitals follow the fee-for-service system and all surgical and treatment procedures are claimed. Despite the aforementioned lack, the NHIS-Senior cohort has a big sample size with a relatively low follow-up loss rate over 13 years due to the nature of the national administrative data. Additionally, because the subjects of the NHIS-Senior were selected by 10% random sampling technique, the NHIS-Senior represents the all population over 60 years of age in South Korea. Thus, it represent all elderly hip fracture patients in South Korea.
In conclusion, male sex increases the risk of death in elderly patients with hip fractures compared to that of matched controls, but the increased risk of death by age in the hip fracture group decreases compared to the increased risk of death by age in the matched controls.
Notes
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant no. HI22C0494).
Ethics approval and consent to participate
The study design and protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Institutional Review Board of the Eulji University Hospital (IRB no. EMC 2019-06-019).
Conflict of interest
No potential conflict of interest relevant to this article was reported.