 |
 |
| jbm > Volume 20(2); 2013 > Article |
|
Abstract
Background
There are few reports on bone mineral density (BMD) changes of axial bones after total knee replacement (TKR) due to severe osteoarthritis (OA) of the knee joint and its results are controversial. The purpose of our study was to measure the BMD changes of hip and spine in patients receiving TKR due to severe OA and to identify clinical factors relating BMD changes.
Methods
Among 66 female patients above 65 years old who underwent TKR due to severe OA and checked preoperative BMD, 52 patients who checked 1 year follow up BMD were enrolled. We investigated the association of the BMD changes with bilaterality of operation, obesity, preoperative knee functional scores, bisphosphonate medication, and diagnosis of osteoporosis.
Results
We found no correlation between BMD changes and bilaterality of operation, obesity, preoperative knee functional scores and diagnosis of osteoporosis. Spine BMD increased in non-treatment and bisphosphonate treatment group but total hip BMD significantly increased in bisphosphonate treatment group.
Conclusions
Bisphosphonate treatment for 1 year prevents early reduction of hip BMD just after TKR regardless osteoporosis diagnosis. We considered that the bisphosphonate medication would be beneficial to prevention of later hip fracture in elderly patient receiving TKR due to severe OA of knee joints.
Osteoporosis and osteoarthritis is a common disease in women over the age of 65 and the recent increase of aging population has increased the number of patients as well as the surgical management cases of both diseases. Because the main risk factors of osteoporosis are aging and low body weight while those main risk factors of knee osteoarthritis (OA) are aging and obesity, these diseases have been considered as having inverse relationship. However, there are lots of patients who have both disease entities. In particular, in the case of patients with severe knee OA, gait disturbance due to pain and reduced activity in the living environment and poor exercise capacity make the bone mineral density (BMD) of the hip area equal or even decrease. The studies about changes of axial BMD in patient who underwent total knee arthroplasty due to severe OA are few and the absence of a consistent consensus. So we measure the BMD changes of hip and spine in patients receiving total knee replacement (TKR) due to severe degenerative OA and identify the correlation with clinical factors such as postoperative bisphosphonate medication, whether bilateral operation, the patient's obesity status, preoperative knee function score, or preoperative diagnosis of osteoporosis.
From January 2007 to May 2010, among 66 female patients over the age of 65 who checked preoperative BMD and underwent total knee arthroplasty due to severe OA, 52 patients who checked follow-up BMD were included. Patients who had a history of brain disease, metabolic bone disease, rheumatoid arthritis and received knee or hip surgery in the past were excluded. There were no patients who used the walking aids, such as crutch or cane because of the knee joint pain after 3months of operation.
BMD at the lumbar and hip region were measured by dual energy X-ray absorptiometry (DXA) with supine position. The bone density of the lumbar region (L1-L4), left femoral neck and left total hip density were measured.[1] Postoperative BMD was measured by same machine and same way. Osteoporosis is defined by a T-score -2.5 or less and osteopenia is defined by a T-score -2.5 between -1 at the lumbar, femoral neck and total hip region whichever is lowest according to the World Health Organization (WHO) international reference standard.[2] Obesity ranges are determined by using weight and height to calculate a number called the body mass index (BMI, kg/m2). A patient who has a BMI between 18.5 and 25 is considered normal and a patient who has a BMI of 25 or higher is considered obese. Preoperative knee functional score was evaluated by the criteria of the American Knee Society respectively.[3] We consider the bilateral operation case if both knee were operated at the same time or within 3months separately, meaning we excluded the cases which both knee were operated more than 3 months period separately.
Descriptive statistics were calculated to determine the demographic and clinical characteristics of patients. Comparison of variables between differences in BMD related to the clinical conditions was tested by using student t-test. Statistical analyses were conducted using SPSS (SPSS Inc., Chicago, IL, USA) for window version 12.0 and statistical significance was accepted for P value of <0.05.
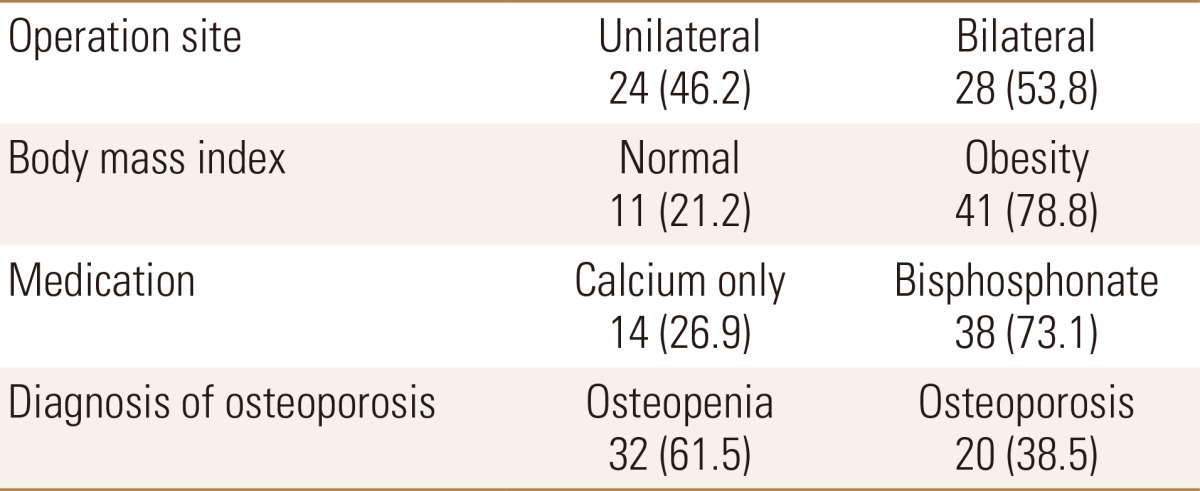
52 patients participated in this study; the average age was 70.2±3.7, the average weight was 62.0±7.9 kg and the average height was 151.0±5.7 cm, the average BMI was 27.2±2.8 and the average functional knee score was 53.4±14.1. There was no significant changes of spine, femur neck, total hip BMD between preoperative and 1 year after the operation (Table 1). Mean follow up period was 2.2 years. There were 28 cases (53.8%) in which the patient received simultaneous bilateral knee surgery, and there were 41 (78.8%) patients who were obese. There were 38 (73.1%) patients who took bisphosphonate medication. Finally, there were 32 (61.5%) cases in which the patients had low bone density, and 20 (38.5%) cases in which the patients were diagnosed with osteoporosis (Table 2).
There are no significant BMD changes to the patients one year after the operation whether they received bilateral knee operation or not, additionally, their obesity level, preoperative knee function score, and preoperative diagnosis for osteoporosis did not matter as well. However, in the bisphosphonate treatment group, total hip BMD was significantly increased compared to the non-treatment group. The spine BMD were increased in both the treatment and the non-treatment group (0.045 g/cm2 and 0.036 g/cm2). Furthermore, the femur neck and total hip BMD were increased in the treatment group (0.006 g/cm2, 0.017 g/cm2) while they were decreased in the non-treatment group (-0.012 g/cm2, -0.020 g/cm2) (Table 3).
Patients with OA of knee joints, in most cases, have relatively higher BMD. OA and osteoporosis have been recognized as inverse relationship to each other because the main risk factors of osteoporosis are aging and low body weight while those of knee OA are aging and obesity.[4,5] However, depending on the patient's age, lifestyle and environments, both diseases may be present simultaneously, especially in cases with long term disability due to OA.[6] Hannan et al.[7] reported mean femoral BMD at the proximal femur sites with lower grades of knee OA to be 5-9% high also compared to those with no knee OA and mean femoral BMD in those with grade 4 OA was not higher than in those with no OA. The authors checked both side hip BMD of patient with severe OA and reported that patients had a lower hip BMD on the symptomatic knee side compared with that of the contralateral hip and hip BMD was positively correlated with grade of radiographic change and negatively correlated with knee functional score.[8] Lingard et al.[9] investigated the prevalence of osteoporosis in patients with severe hip and knee OA awaiting joint arthroplasty and reported that the overall rate of osteoporosis was 23% and 43% of patients would have been classified as osteopenia. In our study, there were 32 cases (61.5%) of patients having low bone density, and 20 cases of patients diagnosed with osteoporosis. Labuda et al.[10] reported that osteoporosis is common in the osteoarthritic arthroplasty population, with a prevalence at least equal to that in the general population and suggested that osteoporosis assessment is needed in patients undergoing a joint replacement.
There are many studies about BMD changes regarding the periprosthetic region after total joint replacement, but studies about BMD changes of axial bone after total joint replacement in patients with OA are limited. Gazdzik et al. [11] reported that a decrease in BMD was observed in all determined regions within one year after the surgery and the most significant BMD decrease at the periprosthetic region was observed in the period between 5-12 weeks after the knee joint arthroplasty, the result furthermore shows increased bone resorption and decreased motor activity of the patients. So they recommended early patient rehabilitation and loading of the operated extremity. Ishii et al.[12] investigated the relationship between TKR and BMD in the same and opposite hips and reported that there was no statistical difference among preoperative, 6 months, 1 year, 2 years after TKR and 45% of the hips on the operative side and 59% of the hips on the non-operative side at 2 years after TKR had higher BMD than preoperative levels. However, Soininvaara et al.[13] checked the BMD in the proximal femur and contralateral knee at one year after TKR and reported neither the hip nor the non-operated knee BMDs increased and concluded that improved mobility after TKR does not improve the effects of preoperative disuse associated with bone loss in the short term. However, in our study, the spine BMD was increased and hip BMD was decreased in non-treatment group at 1 year after TKR.
Studies concerning the relationship between OA and fractures by Bergink et al.[14] investigated the association between prevalent radiographic OA of the knee and incident vertebral and non-vertebral fracture and reported that the knee OA is associated with an increased risk of incidental vertebral and non-vertebral fracture, independent of BMD and parameters of postural stability. Arden et al.[15] reported prevalent knee pain was associated with an increased risk of falling (hazard ratio [HR] 1.26. 95% confidence interval [CI] 1.17-1.36) and hip fracture (HR 2.0 95% CI 1.18-3.37). And they suggested knee pain and OA should be regarded as independent risk factors for fracture.
Joshi et al.[16] reported 4 cases of ipsilateral fracture of the femoral neck after TKR. They explained possible mechanisms of fractures are due to changes in the weight bearing axis of the extremity and poor mobility and weakened bones. So they suggested graduating weight bearing, treating osteoporosis and using less constrained devices may avoid stress fracture of the femoral neck after TKR. Prieto-Alhambra et al.[17] investigated changes of hip fracture rate before and after TKR due to OA and reported hip fracture rates were insignificantly reduced before the operation but, in the year after TKR, relative risk increased significantly up to 1.58 and then declined to equal by 3 years compared with controls.
Recently, bisphosphonate are being prescribed as first choice drug for osteoporosis. And common mechanisms of failure of TKR are represented by aseptic loosening, infection, and instability. Biologic mechanisms related aseptic loosening are large amount of activated macrophages, high concentration of specific cytokines, and presence of bone resorption by osteoclasts.[18] Carulli et al.[19] proposed the use of bisphosphonate in patients undergoing a joint arthroplasty to reduce the progressive bone loss at the counterface between components and bone, to improve implant survival, and to prevent loosening. Hence, bisphosphonate treatment after TKR not only helps strengthen the osteoporotic bone but it also prevents aseptic loosening of implants. Wang et al.[20] evaluated the long term effects of bisphosphonate on periprosthetic BMD changes after TKR. They reported BMD increased at six and 12 months after TKR but no significant difference was noted after thirty-six months. Lee et al.[21] reported that BMD declined in more than half of the patients, even though they took the bisphosphonate treatment for only 1 year after TKR, this decline was significant in bilateral TKR patients. Moreover patients undergoing bilateral TKR, who had more severe OA at baseline had a lower BMD response after 2 years of bisphosphonate treatment, compared with patients with less severe unilateral knee OA who underwent unilateral TKR.[22] However, In our study, in bisphosphonate treatment group, total hip BMD was significantly increased compared to non-treatment group regardless of operation sites whether unilateral or bilateral and osteoporosis diagnosis. Prieto-Alhambra et al.[23] assessed the effect of bisphosphonate use on post TKR fracture risk and reported that the HR associated with bisphosphonate therapy after TKR was 0.5 in non-fractured patients previously and 0.45 in subjects with osteoporotic and with other previous fracture. This suggested bisphosphonate treatment after TKR reduced the risk of fracture by 50-55%.
Spine BMD increased in both bisphosphonate treatment and non-treatment groups but total hip BMD significantly increased in bisphosphonate treatment group only. Bisphosphonate treatment for 1 year prevents early reduction of hip BMD just after TKR regardless of osteoporosis diagnosis. These results considered bisphosphonate medication after TKR would be beneficial to the prevention of later hip fracture in elderly patients who suffer from severe OA of the knee joints and underwent total knee arthroplasty.
References
1. Khan AA, Colquhoun A, Hanley DA, et al. Standards and guidelines for technologists performing central dual-energy X-ray absorptiometry. J Clin Densitom 2007;10:189-195.


2. National Osteoporosis Foundation. Clinician's guide to prevention and treatment of osteoporosis. Washington, DC: National Osteoporosis Foundation; 2010.
3. Rorabeck CH, Bourne RB, Nott L. The cemented kinematic-II and the non-cemented porous-coated anatomic prostheses for total knee replacement. A prospective evaluation. J Bone Joint Surg Am 1988;70:483-490.


4. Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol 1988;128:179-189.



5. Raisz LG. Local and systemic factors in the pathogenesis of osteoporosis. N Engl J Med 1988;318:818-828.


7. Hannan MT, Anderson JJ, Zhang Y, et al. Bone mineral density and knee osteoarthritis in elderly men and women. The Framingham Study. Arthritis Rheum 1993;36:1671-1680.


8. Hahn MH, Ahn JY, Lee KS. Bone mineral density differences of both hips in women with knee osteoarthritis over the age of 65. Korean J Bone Metab 2010;17:87-93.
9. Lingard EA, Mitchell SY, Francis RM, et al. The prevalence of osteoporosis in patients with severe hip and knee osteoarthritis awaiting joint arthroplasty. Age Ageing 2010;39:234-239.



10. Labuda A, Papaioannou A, Pritchard J, et al. Prevalence of osteoporosis in osteoarthritic patients undergoing total hip or total knee arthroplasty. Arch Phys Med Rehabil 2008;89:2373-2374.



11. Gazdzik TS, Gajda T, Kaleta M. Bone mineral density changes after total knee arthroplasty: one-year follow-up. J Clin Densitom 2008;11:345-350.


12. Ishii Y, Yagisawa K, Ikezawa Y. Changes in bone mineral density of the proximal femur after total knee arthroplasty. J Arthroplasty 2000;15:519-522.


13. Soininvaara TA, Miettinen HJ, Jurvelin JS, et al. Bone mineral density in the proximal femur and contralateral knee after total knee arthroplasty. J Clin Densitom 2004;7:424-431.


14. Bergink AP, van der Klift M, Hofman A, et al. Osteoarthritis of the knee is associated with vertebral and nonvertebral fractures in the elderly: the Rotterdam Study. Arthritis Rheum 2003;49:648-657.


15. Arden NK, Crozier S, Smith H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Rheum 2006;55:610-615.


16. Joshi N, Pidemunt G, Carrera L, et al. Stress fracture of the femoral neck as a complication of total knee arthroplasty. J Arthroplasty 2005;20:392-395.


17. Prieto-Alhambra D, Javaid MK, Maskell J, et al. Changes in hip fracture rate before and after total knee replacement due to osteoarthritis: a population-based cohort study. Ann Rheum Dis 2011;70:134-138.


18. Shanbhag AS. Use of bisphosphonates to improve the durability of total joint replacements. J Am Acad Orthop Surg 2006;14:215-225.


19. Carulli C, Civinini R, Matassi F, et al. The use of anti-osteoporosis drugs in total knee arthroplasty. Aging Clin Exp Res 2011;23:38-39.

20. Wang CJ, Wang JW, Ko JY, et al. Three-year changes in bone mineral density around the knee after a six-month course of oral alendronate following total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am 2006;88:267-272.


21. Lee JK, Lee CH, Choi CH. QCT bone mineral density responses to 1 year of oral bisphosphonate after total knee replacement for knee osteoarthritis. Osteoporos Int 2013;24:287-292.



- TOOLS
-
METRICS

-
- 8 Crossref
- 0
- 3,708 View
- 13 Download
- Related articles
-
Age-related Bone Mineral Density of Korean Women in Taegu1996 April;3(1)
Bone Mineral Density of Korea Women using XR-36 1995 April;2(1)
Bone Mineral Density and Related Factors in Middle Aged Men1997 November;4(2)
Normative Bone Mineral Density by Digital X-ray Radiogrammetry in Korean Women2003 November;10(2)





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



