A First Case of Osteomesopyknosis in Korea
Article information
Abstract
Osteomesopyknosis is a rare sclerosing bone disorder of autosomal dominant inheritance. We report a first case of osteomesopyknosis in Korea. A 16-year old girl complained of diffuse back pain for 1 year. We performed physical examination, biochemical investigations and imaging studies. A radiograph of spine revealed rugger-jersey vertebra and sandwich vertebra. Bone specific alkaline phosphatase, osteocalcin and C-terminal telopeptides of type I collagen were normal. Only an axial skeleton involvement was shown on the whole body bone scan. This patient was diagnosed to have osteomesopyknosis. Osteomesopyknosis is characterized by normal level of bone turnover marker and an axial bone involvement. Osteomesopyknosis can be occurred in Korea and needs to be considered when patients, especially young patients, suffer from back pain and have only axial osteosclerosis.
INTRODUCTION
Osteomesopyknosis is rare and a benign osteosclerosis of autosomal dominant inheritance. It was first described by Simon et al.[1] at 1979. The authors reported one patient having a benign axial osteosclerosis without high level of alkaline phosphatase (ALP). One year after, Maroteaux[2] reported five members of four different families and named osteomesopyknosis for a sclerosing axial bone disease with autosomal dominant inheritance which has a good prognosis. Skeletal involvement in osteomesopyknosis is confined to the axial spine, pelvis, and proximal part of the long bone. Osteomesopyknosis is benign disorder and does not cause any deformity, fracture and mental retardation.[3,4] There are no abnormal findings in biochemical analysis.[3,5] Thus, it is usually diagnosed incidentally during radiologic examination when young patients suffer from back pain.[3,4,5] Here, we present the first reported case of osteomesopyknosis in Korea.
CASE
A 16-year old girl visited to orthopedic clinic at Daegu Fatima Hospital due to a history of diffuse back pain for 1 year. Back pain was aggravated when she kept sitting or standing for a long time. Spine X-ray was taken which showed sclerotic change of spine endplate and pelvic bone. Rugger-jersey vertebra and sandwich vertebra was shown (Fig. 1). This girl was referred to Department of Endocrinology and Metabolism at Daegu Fatima Hospital for evaluation of osteosclerosis.

Radiography of spine showing bands of sclerosis at the vertebral end plates and sclerotic change at pelvic bone. (A) Lateral radiograph of thoracic-lumbar spine (B) Lateral radiograph of lumbosacral spine (C) Anterior-posterior radiograph of the lumbosacral spine.
The patient's blood pressure was 120/90 mmHg and her heart rate was 88 beats/min. Her weight was 63 kg and height was 160.3 cm. The results of a physical examination were unremarkable. There was no tenderness, redness and heatness on her back. Back mobility was normal and kyphoscoliosis was not observed. She had a normal stature and no history of fractures. On laboratory examination, liver function and renal function was normal. 25-hydroxy-vitamin D (25-[OH]D) was 7.2 ng/mL (normal range 30.1 to 100.0 mg/mL). 1,25-(OH)D was 27.88 pg/mL (normal range 19.6 to 54.3 pg/mL). Ten point one mg/dL calcium (normal range 9.0 to 11.0 mg/dL), 3.7 mg/dL phosphate (normal range 2.3 to 4.7 mg/dL), 31.7 pg/mL intact parathyroid hormone (normal range 12 to 88 pg/mL) and 5 U/mL rheumatoid factor (normal range 0 to 14 U/mL) were checked. Thyroid stimulating hormone level was 0.484 µIU/mL (normal range 0.7 to 6.4 µIU/mL), but serum free T4 was normal.
In order to identify the cause of osteosclerosis, we checked born turnover markers. Bone specific ALP was 19.11 U/L (normal range 11.6 to 42.7 U/L), osteocalcin was 15.76 ng/mL (normal range 11.0 to 46.0 ng/mL) and C-terminal telopeptides of type I collagen was 0.265 ng/mL (normal range 0 to 1.008 ng/mL). All of these markers were within normal limit.
Assessment of the extent of bone involvement is an important clue to differentiate osteosclerosis. Skull X-ray did not show any abnormality (Fig. 2). Both rib series were normal. Long bone, such as tibia, fibula and humerus had normal bony structure. There was no sclerotic change. To check the involvement of whole body bony structure, bone scan was taken. On whole body bone scan with Tc-99m hydroxymethylene diphosphonate (HDP) image (Fig. 3), there was suspiciously increased uptake in vertebra. And normal uptake was observed at growth plate area.
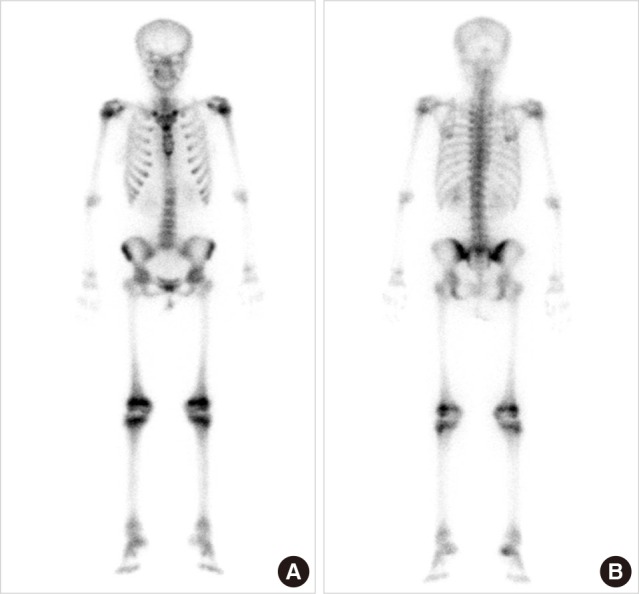
Whole body bone scan with Tc-99m hydroxymethylene diphosphonate (HDP) showing suspiciously increased uptake in vertebra and normal uptake at growth plate area. (A) Anterior image (B) Posterior image.
There was no evidence of increased bone turnover marker and only an axial skeleton involvement was shown on the whole body bone scan. These findings were compatible with osteomesopyknosis. Her mother did not have osteosclerotic lesion in spine radiograph. She has no father, sister or brother. So we could not perform further radiologic investigation of her family.
DISCUSSION
Osteomesopyknosis is a very rare sclerosing bone disorder. Only a few cases were published, the prevalence and pathogenesis are not known. As far as we know, this is the first case in Korea.
The characteristic finding of osteomesopyknosis is osteosclerosis confined to axial skeleton such as spine, pelvis and proximal part of long bone.[6] The radiographic finding of osteomesopyknosis is diverse. Osteosclerosis can be observed in the vertebral end plates like bands of sclerosis,[7] multiple patchy areas is possible.[8] If multiple patchy areas are shown, metastatic disease should be considered. This finding was not shown in our patient. Thus, we did not consider bone neoplasia or metastatic disease. Rugger-jersey spine, the major radiologic finding in our case, can be seen in autosomal dominant osteopetrosis (ADO). So, osteomesopyknosis must be distinguished from ADO. ADO is rare inherited bone disorder characterized by skeletal densification caused by in effective osteoclast-mediated bone resorption. There are two subtypes in ADO on the basis of radiological and clinical differences.[9] Both type of ADO involves a cranial bone. Type I ADO shows an enlarged thickness of the cranial wall and the sclerosis of the skull in Type II ADO is most striking at the base. Clinically, bone pain, recurrent fractures, back pain, and degenerative arthritis can be presented in ADO. Cranial nerve compression is common in type I ADO. In our case, there was no abnormality in skull X-ray and no symptom except back pain.
In the Paget's disease of bone characterized by an accelerated rate of bone remodeling, bone specific ALP is usually elevated and pagetic changes in bone can be seen skull, spine, pelvis, and long bones of the lower extremities.[10] Our patient had normal bone specific ALP level and only axial skeletal sclerosis. This patient had vitamin D deficiency. In this state, osteomalacia and rickets can be occurred. The key findings of rickets, an impeded growth and deformity of the long bones,[11] were not observed. Biochemical abnormalities including calcium, phosphate and ALP level found in osteomalacia and rickets[12] was not shown. Axial osteomalacia mainly involves axial skeleton and presents usually in middle-aged patients.[13] And it can have normal level of bone biochemical parameters.[14] A dense, coarsened, and sponge-like appearance on radiographs is a distinctive finding of axial osteomalacia.[15] In our case, there were no characteristics of axial osteomalacia on radiography. Although the patient had subclinical hyperthyroidism, thyrotoxicosis is known to relate with reduced bone density and osteoporosis.[16]
Osteomesopyknosis is known to have autosomal dominant inheritance, there are reported cases that did not show radiological changes in the parents of the patient.[1,2,4] Thus, osteomesopyknosis is known to a mild form of hereditary osteosclerosis. We could not identify hereditary manner because of lack of her family.
Osteosclerosis is an elevation in bone density and shown as an increased opacity on a radiography. There are many diseases that lead to bony sclerosis such as osteopetrosis, Paget disease and osteomalacia. Differential points are inheritance pattern, age at onset, commonly affected sites, combined abnormality and etc.[17] Osteomesopyknosis is characterized by normal level of bone turnover marker and an axial bone involvement. Osteomesopyknosis has normal life expectancy and does not lead any deformity, fracture and mental retardation.[3,4] So it is very important to differentiate other cause.
In Asia, there are only three Japaness case reports.[7] Our case is the fourth case in Asia and the first Korean case. As osteomesopyknosis is benign disease, if patient has no symptom, this disease can be overlooked. So, the prevalence of osteomesopyknosis can be greater than we expected. In conclusion, Osteomesopyknosis can be occurred in Korea and needs to be considered when patients, especially young patients, suffer from back pain and have only axial sclerosis.
Notes
No potential conflict of interest relevant to this article was reported.
