Patient Perception on Osteoporosis in Korean Female Patients with Osteoporosis
Article information
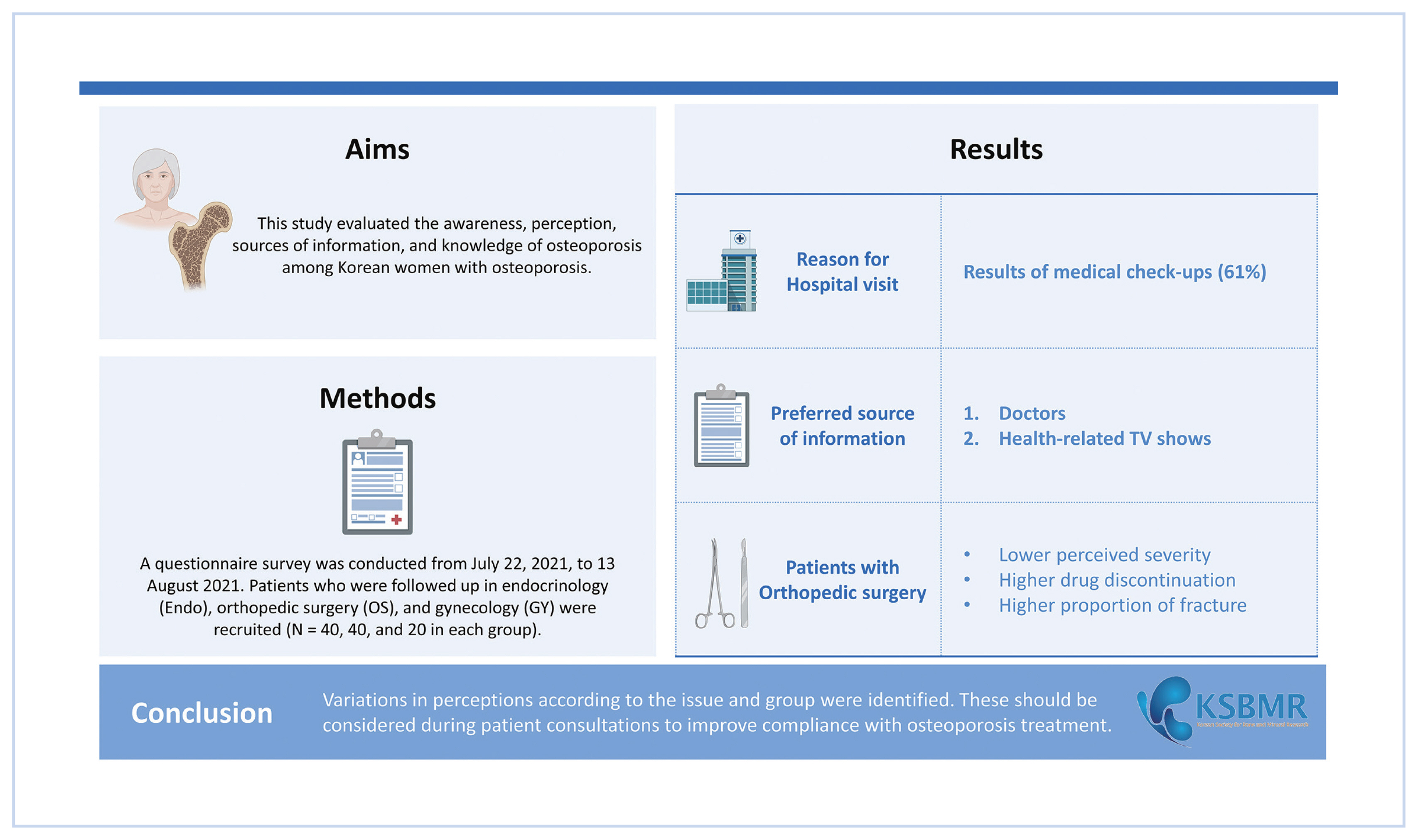
Abstract
Background
Patient perception is a key element in improving compliance with medications for osteoporosis. This study evaluated the awareness, perception, sources of information, and knowledge of osteoporosis among Korean women with osteoporosis.
Methods
A questionnaire survey was conducted from July 22, 2021 to 13 August 2021. Patients who were followed up in endocrinology (Endo), orthopedic surgery (OS), and gynecology (GY) were recruited (N=40, 40, and 20 in each group). Patients were allocated according to their age, as follows: 15, 15, and 10 patients in their 60s, 70s, and 80s for Endo and OS, and 10 and 10 patients in their 60s and 70s for GY. The questionnaire was composed of the following topics: patient journey to the hospital, drug-related issues, communication with medical doctors, patient knowledge, and sources of information about osteoporosis.
Results
The results of medical check-ups were the most common reason for patient visits to the hospital for an initial diagnosis of osteoporosis (61%). A knowledge gap regarding mortality, refracture, and drug-induced osteoporosis was observed. Doctors were the most preferred and trustful source of information, while health-related TV shows were the second most common source of information. Patients with OS reported lower perceived severity and higher drug discontinuation, along with a higher proportion of fractures, as the initial reasons for hospital visits for osteoporosis.
Conclusions
Variations in perceptions according to the issue and group were identified. These should be considered during patient consultations to improve compliance with osteoporosis treatment.
INTRODUCTION
Osteoporosis is the most common skeletal disease in humans [1] causing fragility fractures, that result in decreased functional recovery and increased mortality. The disability associated with fragility fractures in the population is comparable to that of lung cancer, chronic obstructive pulmonary disease, and ischemic stroke.[2] Therefore, treatment of osteoporosis for the prevention of fragility fracture is one of the most important public health issues worldwide.
Osteoporosis treatment has proven its effectiveness in preventing fragility fractures reducing vertebral fractures by up to 70% and hip fractures by up to 53%.[3,4] Given the chronic nature and prolonged treatment required for this disease, drug compliance is essential for successful treatment.[5] However, adherence to osteoporosis medications is known to be suboptimal, varying from 34% to 75% in the first year of treatment [6,7] and persistence levels at 1 year were reported to be between 18% and 75%.[8] This suboptimal adherence and persistence not only lead to increased fracture rate but also result in worse health outcomes.[9,10]
Therefore, research aimed at improving compliance must be prioritized.[5] Various factors including dosing requirements, medical insurance impediments, medication, costs, side-effects of medications, and patient-physician rapport are mentioned,[11,12] but their effect on compliance is not fully understood. Recently, patient perception has been found to predict adherence to medication in a variety of chronic conditions [13] including osteoporosis. Lowered perceptions of the risks of osteoporosis could contribute to medication nonadherence.[14,15] Patients’ beliefs about their perceived need for medication, concerns about medication, experience of side effects, and the inconvenience of dosing regimens are all associated with nonadherence.[16,17]
Therefore, healthcare providers need to determine the population’s perception and preference towards osteoporosis to plan effective education programs [18] and to improve adherence.[19] However, patient perception of osteoporosis and its treatment has not been extensively studied in the Korean population. This study aims to evaluate the awareness, satisfaction with communication, sources of information, and knowledge of osteoporosis in Korean women with osteoporosis to identify unmet needs and expectations to improve optimal communication for better treatment.
METHODS
1. Study population
This study was conducted from 22 July 2021 to 13 August 2021. Female patients followed up by endocrinology (Endo), orthopedics (OS), and gynecology (GY) departments for osteoporosis in general hospitals in Seoul, Gyeonggi-do, Incheon, and other 4 major cities were enrolled. Eligible patients were interviewed during their regular visits. A total of 100 women were enrolled, and for Endo and OS, 40 patients were enrolled respectively comprising 15 patients in their 60s, 15 patients in their 70s, and 10 patients in their 80s. For the GY clinic, 20 patients were enrolled comprising 10 patients in their 60s and 10 patients in their 70s old resulting in a total of 40 patients in their 60s, 40 patients in their 70s, and 20 patients in their 80s. Patients with a history of dementia were excluded.
2. Patient screening and interview
We conducted quantitative and computer-assisted personal interviews (CAPI) with participants. Before the survey, patients were asked to complete a screening to confirm eligibility for this study including demographics and the presence of diseases, other than osteoporosis, that have been treated for more than 6 months. Once the target number of respondents was reached, further interview was not carried out with the patient. For the enrolled patients, a survey was conducted through one-on-one interviews, each lasting approximately 30 min.
CAPI was composed of the following topics including: Patient Journey to hospital, drug-related issues, communication with medical doctors, patient knowledge, and source of information about osteoporosis. Each topic is composed of the following details.
Patient journey: Trigger of initial hospital visit, age of initial diagnosis of osteoporosis, history of hospital change, and reason for hospital change (multiple choice)
Drug-related: Currently prescribed medication, history of drug change, situation of drug change, history of drug discontinuation, reason for drug discontinuation, perceived difficulty during treatment
Communication: Information by doctor when diagnosed, methods of information delivery, satisfaction level on explanation, reason of dissatisfaction, response to the doctor after feeling dissatisfaction
Patient Knowledge: Self-perceived level of awareness, awareness of osteoporosis symptoms, causes, risk-related and treatment-related, and perceived severity
Source of information: Information channel when diagnosed, preferred information channel, most truthful information channel, additional information required.
3. Statistical analysis
A χ2 test was done to compare the difference between groups (According to department and according to age group) SPSS statistics (version 27; SPSS Inc., Chicago, IL, USA) was used for the analysis. For comparison, a 5-point Likert scale was divided into no (1, 2, and 3) and yes (4 and 5).
RESULTS
1. Demographics of the respondents
Depending on the region, there were 60 patients in Seoul/Gyeonggi/Incheon, 12 in Daejeon/Chungnam, 11 in Busan/Gyeongnam, 9 in Gwangju/Jeolla, and 8 in Daegu/Gyeongbuk. Regarding the highest level of education, 85 patients graduated from high school or less, 3 dropped out of college, 9 graduated from college, and 3 did not respond. Eighty-eight percent of osteoporosis patients had comorbidities with the following prevalence orders: Hypertension>Diabetes>Dyslipidemia. The proportion of patients with comorbidities was highest in Endo (98%) and lowest in GY (75%). Almost all patients with comorbidities were prescribed medication for treatment.
2. Diagnosis and medications for osteoporosis
More than half of the patients (61%) were diagnosed with osteoporosis through regular medical check-ups. By specialty, OS patients showed a higher proportion of joint problems (45%) and/or fractures (35%) which is 2 to 3 times higher than Endo/GY (P<0.05). The 37% of patients changed their hospital for osteoporosis treatment at least one time after osteoporosis diagnosis, and the proportion was notably higher in the age group of 70s (65%) compared to those in their 60s (18%) and 80s (20%) (P<0.01) (Table 1).
Thirty-seven percent of patients had a history of drug change. Patients in OS tended to have more experience of drug change(s) than other specialties (45% vs. 33 and 30%) Most common situation for drug change was their doctor’s recommendation (62%) but in the GY group, patient suggestions for change were 83%. The 14% of patients had experience of stopping medication in the past, and OS patients showed a higher rate of treatment discontinuation than other specialties (23% vs. 8 and 10%) The primary reason for drug discontinuation was ‘insufficient efficacy’ (36%) followed by ‘not enough pain/inconvenience’ (29%) and ‘bothersome’ (29%). The most significant difficulty that patients experienced during treatment overall was the ‘lack of effect’ (23%) (Table 2).
When diagnosed with osteoporosis, the largest number of patients were informed about ‘what osteoporosis is’ (65%), followed by ‘(future) treatment plan and process’ (54%) and ‘current condition and prognosis’ (52%). The majority of patients (77%) were satisfied with their doctor’s explanations but 23% were not satisfied. Among subgroups, patients in OS and those in their 70s showed the lowest satisfaction level compared to other subgroups. The most common reason of dissatisfaction with the doctor’s consultation was ‘too short consultation time (61%)’ followed by ‘too difficult explanation (28%)’ and ‘insufficient explanation (22%)’ When the doctor’s explanation was too difficult or insufficient, only 56% of patients actively responded by asking questions immediately (Table 3).
3. Level of Knowledge of the patients
About half of the patients (55%) perceived that they were well aware of osteoporosis. More than two-thirds of patients mentioned that they are well aware of osteoporosis-related symptoms mentioned in the list. However, 55% of patients did not know that osteoporosis can be developed without any special signs/symptoms. Regarding osteoporosis causes, ‘Aging’ (95%) was perceived as the most common cause of osteoporosis, followed by ‘lack of nutrition’ (91%), ‘family history’ (60%), and ‘drugs’ (51%) were less recognized as causes of osteoporosis. Awareness of osteoporosis treatment was higher than awareness of osteoporosis risk, and issues related to re-fracture and mortality were low. Most groups perceived osteoporosis as a severe disease, but OS patients tended to show lower perceived severity (78% vs. 93 and 95%) (P=0.07) (Table 4).
Most patients gained information through ‘doctor’ (95%) and ‘family/acquaintances’ (53%) when diagnosed with osteoporosis followed by TV health-related shows (27%). The most preferred information channel for new information was ‘doctor’ (68%) followed by TV health-related shows (10%). The most truthful information channel was ‘doctor’ (94%) while TV health-related shows were considered truthful by only 2% of patients. Concerning additional information required by patients, drug-related issues still ranked high, along with information on good exercise (36%) and diet (32%) (Table 5).
DISCUSSION
Although treatment of osteoporosis is known to prevent various fragility fractures by about 50%,[20] compliance to osteoporosis treatment is reported to be low.[8] This study aimed to investigate patient understanding on osteoporosis using a questionnaire. The principal findings of this study are that 61% of patients are diagnosed with osteoporosis through regular medical check-ups and 37% of patients have a history of drug change. In addition, 55% of patients perceived that they were well aware of osteoporosis. Most patients gained information through ‘doctor’ (95%) and ‘family/acquaintances’ (53%) when diagnosed with osteoporosis followed by TV health-related shows (27%).
The most common reason for patients to visit the hospital for the initial diagnosis of osteoporosis was the result of a medical check-up. This finding may be attributed to the increased diagnosis rate of osteoporosis in Korean patients after the inclusion of dual energy X-ray absorptiometry (DXA) in annual medical check-ups for women aged 54 years old since 2007, which is reported to have risen from 29.9% in 2008–2009 to 62.87% in 2016–2017.[21] The significance of this heightened screening test becomes more apparent, given that almost half of our patients (45%) are unaware that osteoporosis has no particular symptoms. Concurrently, efforts should be directed towards improving the quality control of DXA, particularly in medical check-up settings, as even in Metropolitan areas, the quality control of DXA is suboptimal with over 90% of technicians failing to perform monthly quality control.[22]
We identified knowledge gaps in our results. Among risk-related knowledge, items related to mortality were found to be lower than other aspects. The statement “If osteoporosis causes hip bone fractures, 1.5 out of 10 people die within a year” had a 63% response rate, while “The risk of death from a femur fracture equals that of breast cancer, four times higher than that of endometrial cancer” had a 53% response rate. Regarding the shortage of mortality information provided to patients, there are abundant reports on epilepsy patients, and the shortage is considered to stem from the belief that discussing unpleasant subjects with patients induces stress and anxiety or reduces their quality of life.[23–25] However, as most guidelines on epilepsy recommend providing information on mortality to improve patient outcomes,[26] education on mortality should be considered to enhance outcomes in osteoporosis patients. However, as shown in the Risk Communication in Osteoporosis study by Beaudart et al. [27], the importance of perception regarding mortality in osteoporosis patients exhibited high variation across nations, this issue should be explained cautiously taking account of local preferences.
To address these knowledge gaps, the role of physician is the paramount, given that our study identified doctors as the most preferred (68%) and truthful (94%) source of information which is consistent with previous studies.[28–30] However, along with previous study,[31] current satisfaction level with doctor’s explanation was not notably high (77%) and the most common reason for dissatisfaction was “too short consultation time” (61%). This corresponds with findings in earlier research,[32] highlighting the importance of doctors allocating sufficient time to enhance patient compliance. To enhance long-term knowledge, communication should be tailored to the patient’s language taking account of their history, needs and health literacy.[33] Additionally, doctors should recognize that attentive listening is a crucial aspect of ensuring patient satisfaction.[34]
One interesting result worth noting is that TV health-related shows were the second most common information channel when diagnosed and the most preferred information channel after doctors, despite that channel’s low reliability. The delivery of health information through mass media offers the advantage of being relatively easy to understand and provides improved accessibility for individuals with limited access to health information.[35] A study by Kim et al. [36] found that senior citizens in the community primarily obtain health information through mass media, and TV in particular, was identified as the ‘place where the health information content was the most informative and helpful’ and ‘the place where the content was easiest to understand’. Given these insights, it is crucial to improve the reliability of TV show content should be improved, and in this regard, the role of osteoporosis society becomes pivotal.
Between groups, respondents in the OS exhibited a lower perceived severity (not severe 23% vs. 8 and 5%; P=0.07) and a higher drug discontinuation rate (23% vs. 8 and 10%; P=0.131) even with a higher rate of fractures as a reason for the initial visit (35% vs. 15 and 15%; P=0.035). Furthermore, the risk-related knowledge including the risks of morbidity and re-fracture after fracture, was also low in OS group. This observation can be explained by the phenomenon where patients who have sustained previous fractures may not perceive themselves at a higher risk of fracture and attribute the fracture to osteoporosis.[15,37,38] This may be in contrast with the physician’s belief. Therefore, it is important to provide education on the importance of understanding osteoporosis and the increased risk of fracture to patients who have already experienced a fracture. Additionally, since this misperception is known to persist over time,[39] continuous education and close monitoring should be provided to this patient group.
There are some limitations to this study. First, this data is exclusively from Korean patients. However, it is reported that there is substantial variation in patient perception between nations [27] which implies the importance of understanding local preferences as this study aimed to investigate. Second, demographic factors and perception issues were not analyzed in this study. However, it is known that demographic factors have not consistently predicted patient perceptions,[39,40] so the actual incidence or tendency may be a more crucial factor when providing care. Third, due to the small sample size, we could not conclude some important points in this study including patient engagement, i.e., which showed higher engagement in the GY group and lower engagement in age over 80. Based on this finding, additional large-volume studies should be considered in the future.
Variations in perception according to issues and groups were identified in this study. These should be taken into consideration in patient consultation to improve compliance with osteoporosis treatment.
Notes
Ethics approval and consent to participate
This study was conducted exclusively with secondary data without identification of subjects, and its procedures are in accordance with the principles of ethics in research involving human beings. Thus, the study was waived from formal review and informed consent by the institutional Research Ethics Committee. However, the study was conducted according to the Helsinki declaration and good clinical practice.
Conflict of interest
Interview and data collection were supported by AMGEN®. No potential conflict of interest relevant to this article was reported.