Mortality Rate and Outcomes of Omicron Variant Positive Patients with Osteoporotic Fractures: A Retrospective Study
Article information
Abstract
Background
During the lockdown period associated with the coronavirus disease 2019 (COVID-19) pandemic, increased mortality rates among patients with COVID-19 have been reported. This study aimed to analyze the mortality rate of osteoporotic hip fractures in patients who were COVID-19-positive after the lockdown during the Omicron period.
Methods
A retrospective study was performed with 194 patients who were aged 70 years or more and diagnosed with osteoporotic hip fracture. The patients were divided into two groups according to their COVID-19 diagnoses. Surgery was performed within 10 days of diagnosis. Age, sex, past medical history, time until surgery, postoperative complications, and the primary outcome of mortality rate at 30 and 90 days were analyzed.
Results
Among the 194 patients, 13 and 181 were in the COVID-19-positive and negative group, respectively. The total, 30-day, and 90-day mortality rates in the control and COVID-positive group were 11% and 0% (P=0.368), 1.7% and 0% (P=1.000), and 5.0% and 0% (P=1.000), respectively. No significant differences were observed in age, sex, history, time to surgery, postoperative complications, or postoperative mortality. In 1:1 propensity score matching, the time to surgery was 5.34 days in patients who were COVID-19-positive, and 3.00 days in patients who were COVID-19 negative, with no statistical significance (P=0.09). Age, sex, medical history, postoperative complications, and postoperative mortality were not significantly different between the groups.
Conclusions
Regardless of the COVID-19 diagnosis, surgical treatment without delay is believed to result in positive outcomes in older patients with osteoporotic hip fractures, as no significant differences in mortality rate and respiratory complications were observed between patients who were COVID-19-positive and those who were COVID-19 negative.
INTRODUCTION
The Coronavirus disease 2019 (COVID-19) pandemic, caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in December 2019 in Wuhan, China. The impact of this disease was devastating, as the World Health Organization (WHO) declared a public health emergency on January 30, 2020. As of April 2023, more than 760 million global cases and approximately 6 million global deaths have been confirmed.[1] Among various variants of COVID-19, the Omicron variant, became the dominant variant worldwide in November 2021, with South Korea not being an exception.[2,3] The first reported Omicron subvariants were the BA.1 and BA.2 at the end of 2021, followed by the emergence of the subvariant BA.5 on April 4, 2022, which became the most frequently encountered variant by November 2022.[2–4]
Lockdown was implemented in many nations during the initial emergence of the pandemic to prevent the spread of COVID-19, and for this reason patients worldwide had a difficult time accessing medical services, which made prompt treatment challenging, including patients with severe injuries such as hip fractures. Osteoporotic hip fracture in the elderly is a serious orthopedic injury that usually requires early intervention for better functional outcomes as well as preventing perioperative complications and mortality.[5] Therefore, patients with hip fractures who test positive for COVID-19 pose a particular challenge, as patients who require isolation from COVID-19 are at higher risk of developing multi-organ complications, which is reported to cause a higher perioperative mortality rate in elderly hip fractures.[6]
There are many reports on the increased mortality of osteoporotic hip fracture patients during the COVID-19 lockdown period, however there have not been studies done during the Omicron dominant period, which was the dominant variant in South Korea since 2022. This study aims to report an up-to-date mortality rate of osteoporotic COVID-19 elderly patients who have undergone surgery at a tertiary institute in South Korea during the Omicron variant dominant period. This is the first paper to report on the mortality rate of COVID-19 positive osteoporotic hip fracture patients during the Omicron dominant period, to the author’s knowledge.
METHODS
A retrospective study was done on all patients undergoing hip fracture surgery between January and December 2022. Patients were aged 70 and over, with osteoporotic hip fracture. Osteoporotic fracture was defined as an injury that occurs from low-level or low-energy trauma, which would not ordinarily result in a fracture, according to the National Institute for Health and Care Excellence clinical guidelines. Operation is done by a single surgeon at a single tertiary institute in South Korea. The 194 patients diagnosed with femoral neck and intertrochanteric femur fracture underwent surgery with bipolar hemiarthroplasty or proximal femur nailing. This study was approved by the institute’s Institutional Review Board center.
All patients were tested for COVID-19 using the 2019-NCOV SD M10 SARS-CoV-2 and 2019-NCOV EXPERT SARS-CoV-2 real-time reverse transcription–polymerase chain reaction test, and patients who tested positive were admitted into isolation wards. Once the patient was isolated, surgery was done without delay within 10 days after the diagnosis. Age, sex, body mass index (BMI), a past history that could affect the patient’s mortality,[7,8] diagnosis, type of anesthesia and surgery were all documented. All-cause mortality at 30-day and 90-day were analyzed as the primary outcomes. All patients were followed up for at least 90 days and the mortality cases were confirmed with the electronic medical record and the national insurance database. The time from injury to surgery, admission to surgery, and the total admission period were measured. Postoperative complications independent from the expected recovery after surgery, and postoperative intensive care unit (ICU) care were the secondary outcomes that were analyzed.
The analysis was conducted using SPSS version 25.0 (IBM Corp., Armonk, NY, USA) and R 4.2.2 (The R foundation, Vienna, Austria). The student’s t-test was performed for continuous variables, and χ2 tests were used for categorical variables. Since there was a large difference in the number of subjects between the COVID-19 group and the control group, 1:1 propensity score matching (PSM) was used. The factors considered to be the risk factors affecting hip fracture mortality such as age, sex, history of coronary artery obstructive disease (CAOD), and chronic kidney disease (CKD) were used to estimate the propensity score.[9] Each COVID-19-positive patient was then matched to a control subject based on propensity score. All of the statistical significance was defined as P-value less than 0.05.
RESULTS
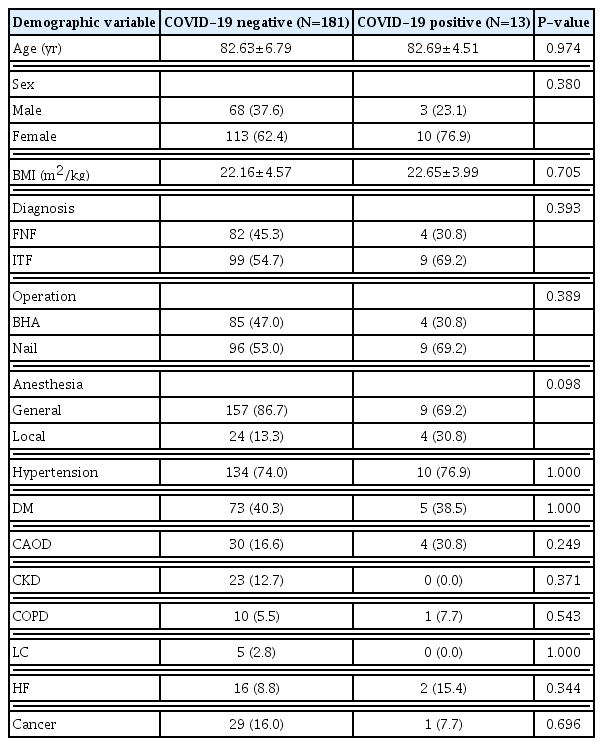
Out of 194 patients diagnosed with osteoporotic hip fractures who underwent surgery, 13 patients tested positive for COVID-19 (6.7%) and 181 patients tested negative (93.3%). Between the COVID-19-positive and negative groups the average age was 82.69±4.51 and 82.63±6.79 (P=0.974), and the average BMI was 22.65±3.99, 22.16±4.57 (P=0.705) respectively, which showed similar values but of no statistical significance. Intertrochanteric fracture (ITF) was more common than femur neck fractures (FNF) in both COVID-19-positive and negative groups with a ratio of 9 (69.2%):4 (30.8%) and 99 (54.7%):82 (45.3%) respectively, which did not hold statistical significance (P=0.393). The surgery method using intramedullary (IM) nail was more common than bipolar hemiarthroplasty (BHA) in both COVID-19-positive and negative groups with a ratio of 9 (69.2%):4 (30.8%) and 96 (53.0%):85 (47.0%) in respectively, which also did not hold statistical significance (P=0.389). Also, comorbidities such as hypertension, diabetes, CAOD, CKD, chronic obstructive pulmonary disease (COPD) liver cirrhosis (LC), heart failure (HF), and cancer all showed no significant difference between the 2 groups (Table 1).
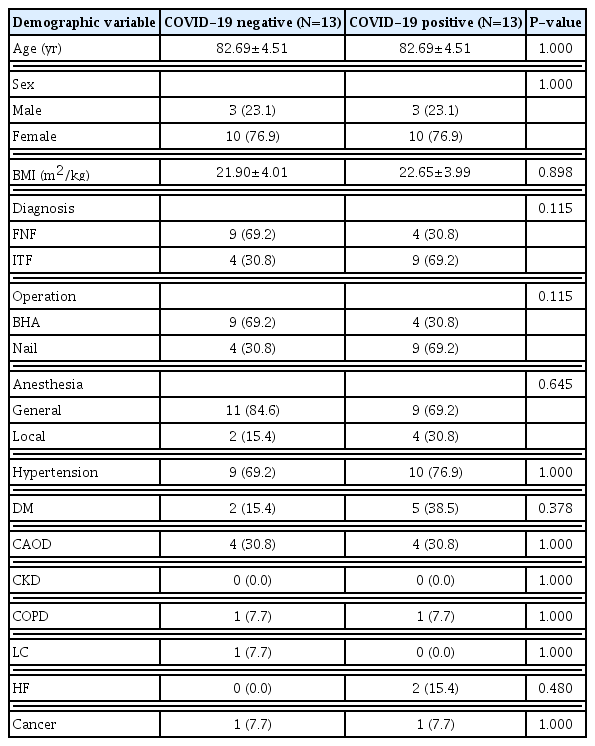
Demographic comparison results after PSM also showed no statistically significant difference between the 2 groups in age (P=1.000), sex (P=1.000), BMI (P=0.898), diagnosis (P=0.115), operation method (P=0.115), type of anesthesia (P=0.645), comorbidities such as hypertension (P=1.000), diabetes mellitus (P=0.378), CAOD (P=1.000), CKD (P=1.000), COPD (P=1.000), LC (P=1.000), HF (P=0.480), and cancer (P=1.000) (Table 2).
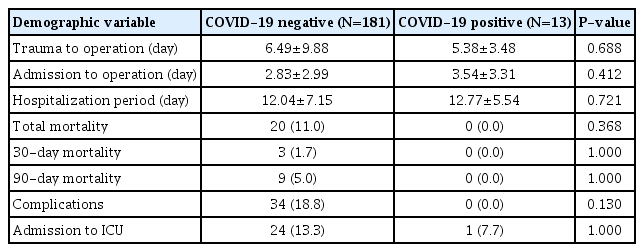
The average days from trauma to operation were longer in the control group compared to the COVID-19-positive group with 6.49±9.88 and 5.38±3.48 respectively, but it did not have statistical significance (P=0.688). However, the days from admission to operation were shorter with 2.83±2.99 and 3.54±3.31 respectively, which also did not have statistical significance (P=0.412). The hospitalization period in the COVID-19 negative and positive groups were 12.04±7.15 and 12.77±5.54 respectively with no significant difference (P=0.721). The total mortality rate, 30-day mortality rate, 90-day mortality rate, complications, and admission to ICU was higher in the control compared to the COVID-19-positive group with 11% and 0% (P=0.368), 1.7% and 0% (P=1.000), 5.0% and 0% (P=1.000), 18.8% and 0% (P=0.130), 13.3% and 7.7% (P=1.000) respectively, showing no statistical significance (Table 3).
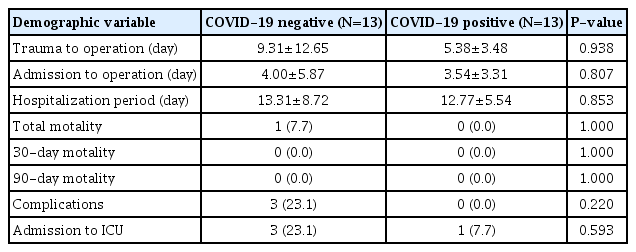
When surgical outcome data was analyzed after PSM, the variables were consistent in having no statistically significant difference between the 2 groups with P-values as follows: trauma to operation (P=0.938), admission to operation (P=0.807), hospitalization period (P=0.853), total mortality rate (P=1.000), 30-day mortality rate (P=1.000), 90-day mortality rate (P=1.000), complications (P=0.220), and admission to ICU (P=0.593) (Table 4).
DISCUSSION
This study showed that there was no significant difference in complications, 30-day and 90-day mortality rates between COVID-19-positive and negative osteoporotic hip patients during the Omicron dominant period in South Korea when surgery was done without delay, within 10 days of isolation period. It is well documented that patients with hip fractures who test positive for COVID-19 are challenging to manage, as quarantine isolation and delay in surgery can keep patients at a higher risk of developing severe complications from the COVID-19 infection, involving various systems such as renal (24.3%), respiratory (18.4%), cardiovascular (12.3%), neurological (4.3%), and gastrointestinal (0.8%).[6] As such, an increased risk of perioperative complications and a weakened immune system may be a contributing factor to the reports of increased mortality rate, increased time to surgery, and longer hospital stays of patients diagnosed with COVID-19.[10,11] Furthermore, fear and anxiety as well as the lockdown itself had restricted physical activities and healthcare access for the elderly, which may have played a role in exacerbation of chronic medical conditions.[12]
In relation to the problems COVID-19 poses, a higher mortality rate in hip fracture patients during the COVID-19 pandemic is well reported. In a national study done in the U.S., the 30-day mortality was 14.6% with COVID-19-positive versus 3.8% for COVID-19-negative, whereas the all-cause mortality for hip fracture surgery was 27.0% in the COVID-19-positive group during the study period.[8] Another study reported that the mortality risk was 3.97 times higher and hospital stays also significantly higher than in patients without COVID-19.[11] Various meta-analyses reported a wide range of COVID-19 hip fracture mortality rates across nations: UK 14.3%, Spain 14.90%, Italy 9.6%, and the USA 6.2%.[13–15]
However, there has been conflicting literature that reported similar mortality rates between the COIVD-19 positive and negative patients who have undergone surgery as well as a recent trend of decrease in mortality rates between the two groups.[16–19] A meta-analysis review done by Tripathy et al. [18] reported that there was no significant difference in the 30-day mortality rate between the pre-pandemic and pandemic periods. Furthermore, the authors reported that there was no difference in time to surgery, length of hospital stay, major complications, and respiratory complications between the two periods. Another study using a nationwide cohort also demonstrated that the mortality rate of hip fracture patients who underwent surgery did not increase in 2020 in South Korea where lockdown was not implemented.[19]
Likewise, this study showed that total mortality, 30-day mortality, and 90-day mortality rates between COVID-19-positive and negative patients showed no significant difference during the Omicron dominant period in South Korea when surgery was done within isolation period. Although the sample size was larger for the COVID-19 negative group, the mortality rates in all three categories were actually higher in the negative group compared to the positive group (total mortality rate 11% vs. 0%, 30-day mortality rate 1.7% vs. 0%, 90-day mortality rate 5.0 vs. 0%), which is contrary to many papers that report a high mortality rate in the COVID-19-positive patients. Additionally, complications, and admission to ICU were also higher in the COVID-19-positive group with no statistical significance (18.8% vs. 0% and 13.3% vs. 7.7% respectively).
There are several reasons that can be proposed for the similar mortality rates of hip fracture patients that undergo surgery between the COVID-19-positive and negative patients. Firstly, most of the previous research has been done during the lockdown period when the Delta strain was dominant. According to WHO, the Delta variant was a potent variant of the COVID-19 which spread more easily and was responsible for more cases and deaths worldwide than the previous strains of viruses.[1] On the other hand, this study collected data during the Omicron-dominant period of 2022 in South Korea, which was after the global lockdown. The Omicron variant has been described as a strain that is less severe than the Delta variant,[1] which may explain the insignificant difference in mortality rates between the COVID-19-positive and negative patients.
Furthermore, these results can be credited to the adoption of improved screening and quality primary and secondary care in hip fracture patients. In Europe, shortages of hospital beds, medical supplies, and healthcare providers during the early COVID-19 pandemic made it difficult for patients with hip fractures to access healthcare, which consequently affected the mortality rate.[15] In this study, screening and planning for surgery was done with minimum delay, as patients underwent surgery within 10 days after COVID-19 diagnosis during their isolation period. Numerous kinds of literature have pointed out the importance of healthcare accessibility and time to operation, as this could affect the clinical outcomes of the patient in mortality, postoperative complications, and recovery from ambulation.[20,21] Likewise, implementation of a protocol to rapidly screen and treat the patient is thought to be essential for favorable clinical outcomes.
Moreover, various countries such as UK, Italy, and the US implemented strict lockdowns, which focused on herd immunity, as the pandemic worsened during the COVID-19 breakout.[22] The lockdown strategy was necessary in certain countries to stop the spread of the virus where there was a shortage in medical supplies, personnel, and facilities to meet the overwhelming number of patients in need.[23–25] On the other hand, several Asian countries such as South Korea, Japan, and China did not practice a full lockdown regulation where people had curfews and were required to stay home. These countries were reported to have lower mortality from the COVID-19 thanks to prompt management and accessible healthcare infrastructure.[26] The strategy of these countries focused on isolating infectious individuals, rather than shutting down the whole community allowing the patients to have easier access to medical care and receive rapid treatment, which could ultimately affect the clinical outcome of patients who require surgery for hip fractures.
This study had several limitations, such as being a retrospective study, having a small sample size, a large difference in sample size between two study groups, and being a single center and single country study. As the study was during on a pandemic period, there was difficulty in pre-planning and having control over the variables to analyze. Also, since the sample size of the COVID-19 group was inherently smaller, the patient composition between the two groups showed differences, which may have influenced the statistical analysis. Although, PSM was utilized to make up for these limitations, further multicenter studies could support the data of similar mortality rates between COVID-19-positive and negative patients who underwent surgery after the global lockdown phase. Despite these limitations, this study brings meaningful data on positive clinical outcomes in COVID-19-positive patients during the Omicron dominant period who were treated without delay.
There was no significant difference in mortality rate and respiratory complications between the COVID-19-positive and negative hip fracture patients who underwent surgery during the Omicron dominant period. It is widely accepted that osteoporotic hip fracture injuries need prompt intervention to improve functional outcomes and reduce perioperative as well as mortality.[5] Therefore, regardless of COVID-19 diagnosis, surgical treatment without delay is thought to bring positive outcomes for elderly patients with osteoporotic hip fractures.
Acknowledgments
The authors would like to thank Professor Tae Hoon Kong in Department of Medical Informatics and Statistics, Yonsei University, for providing assistance with the statistical analysis in this study.
Notes
Ethics approval and consent to participate
This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved.
Conflict of interest
No potential conflict of interest relevant to this article was reported.