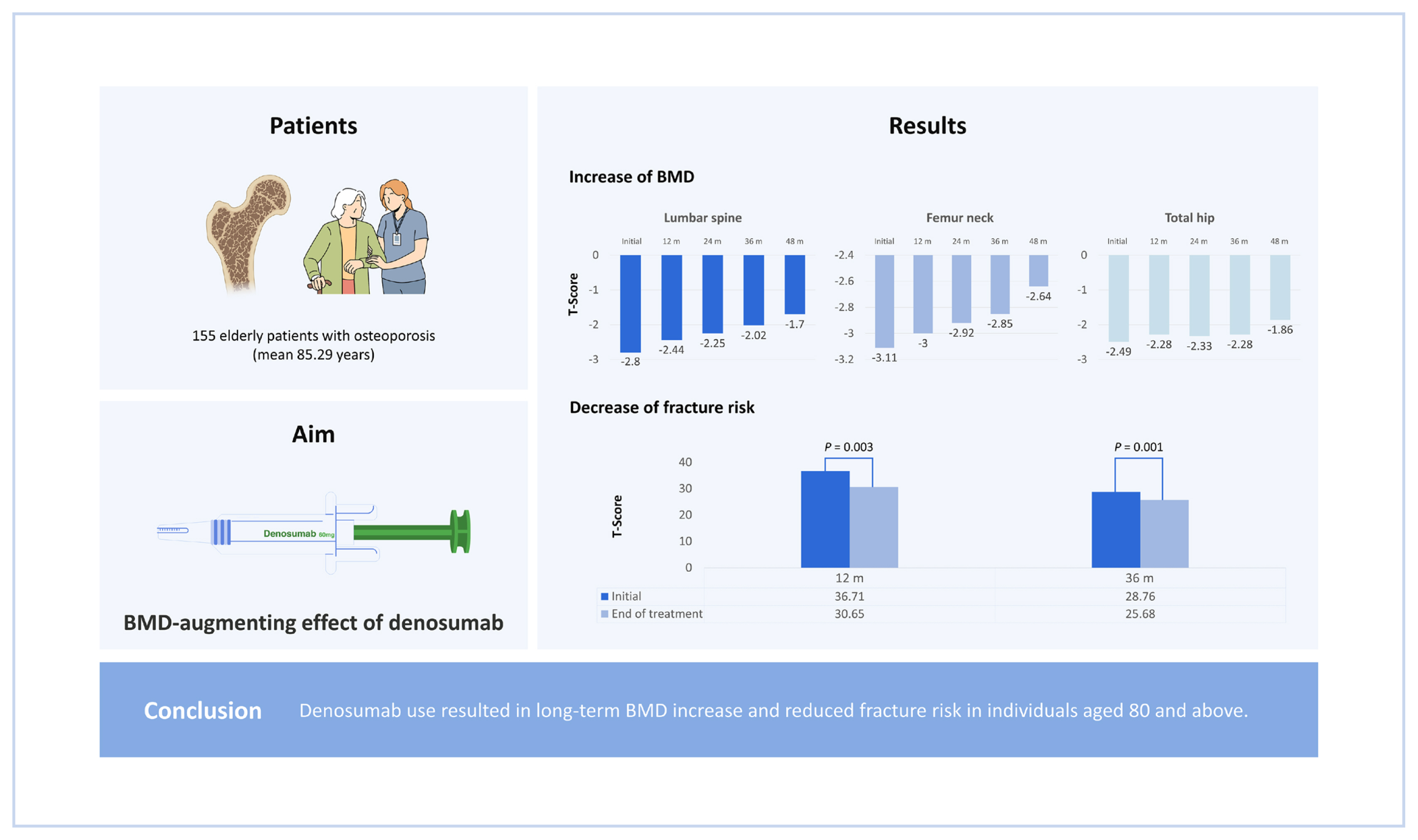
The Effect of Denosumab in Elderly Patients Regarding Bone Density and Fracture Risk
Article information
Abstract
Background
With an aging population, the importance of treating and diagnosing osteoporosis is increasing. Osteoporosis, previously known as a resorptive change primarily related to endocrinological mechanisms, is also being approached as a phenomenon of senile change. Denosumab is gaining popularity among osteoporosis medications due to its ability to increase bone mineral density (BMD) and the economic benefit arising from the 6-month cycle. In line with previous literature, this study aimed to examine the BMD-augmenting effect of denosumab through which it reduces fracture risk in individuals aged over 80 years.
Methods
We reviewed patients who received denosumab between 2018 and 2022 with a minimum clinical observation period of 12 months. BMD was measured every 12 months, and patients were classified per their period of denosumab use. Fracture risk was evaluated using the fracture risk assessment tool (FRAX) and fracture incidence during the observation period were assessed.
Results
Among 155 patients, a significant increase in BMD was observed at 3 sites: the lumbar spine, femoral neck, and total hip (P<0.001, P<0.001, and P=0.001, respectively). The patients were divided according to the length of clinical follow-up they received, and similar results were found in all subgroups. Fracture risk assessment was performed using FRAX and the incidence of fracture events during follow-up. FRAX significantly decreased in all subgroups except those who received 24 months of follow-up (P=0.003, P=0.41, P=0.001 in the 12, 24, and ≥36 months groups, respectively).
Conclusions
Denosumab use resulted in long-term BMD increase and reduced fracture risk in individuals aged 80 and above.
INTRODUCTION
There has been a steep rise in an aging population in Korea and this trend is expected to continue through 2022.[1] According to national statistics, the population aged over 65 years is estimated to be over 9.4 million, which accounts for 17.5% of the total population.[1] This rapid shift in aging has influenced the healthcare sector as new perspectives related to senile changes and the management of osteoporosis are becoming increasingly important. Osteoporosis, if undetected and untreated, increases the risk of hip, spine, and wrist fractures,[2] increasing the length of hospitalization and medical expenses and decreasing survival.[3] Studies on the etiology and pathophysiology of osteoporosis in the senile population are now focusing on the role of decreased sex hormones and other nutritional factors.[4,5] Based on the knowledge of such physiological changes, various medications have been developed to target distinct metabolic pathways of bone metabolism, and these medications are widely used. In several clinical trials, denosumab, a monoclonal antibody-based anti-resorptive drug, was efficacious in reducing the risk of fracture in postmenopausal women.[6,7] Jeong and Ha [8] highlighted the effects of denosumab use in super-elderly patients during the first year of follow-up. Although their study showed increased bone mineral mass during the first year after the initial injection, the clinical efficacy in larger patient groups and the change in fracture risk remained undiscussed.[8]
From this perspective, we devised our study to evaluate the usefulness of denosumab in improving bone mineral density (BMD) after several years of use and its efficacy in lowering the fracture risk assessment tool (FRAX) score, especially in super-elderly patients. We assumed that BMD would significantly increase regardless of the duration of denosumab use.
METHODS
We retrospectively reviewed the records of patients diagnosed with osteoporosis and treated with denosumab between January 2018 and December 2022 at a single center. Patients aged >80 years who received >12 months of clinical follow-up were included in the study. Patients who had to switch from anti-resorptive medication because of dental treatment or vice versa were excluded. A total of 155 patients were enrolled. At the start of treatment, BMD was measured using dual energy X-ray absorptiometry. The FRAX and the presence of recent fractures at the time of the clinical visit were used to evaluate the risk of osteoporotic fractures. BMD was monitored annually after the initial denosumab administration. Patients received 60 mg of denosumab via subcutaneous injection. If the patient was already taking medication to control osteoporosis before denosumab administration, the type of medication and the period of its use were recorded. Oral doses of vitamin D and calcium were administered to the patients unless they experienced gastrointestinal symptoms with their use.
To assess fracture risk reduction, we used the FRAX and evaluated the occurrence of fracture events during the clinical follow-up period. The FRAX, designed by the World Health Organization based on Caucasian data, is used among primary care physicians to assess fracture risk.[9] However, since it is based on Caucasian data, its direct application to people of other races is limited. Further, the FRAX does not include many important clinical factors, including the degree of daily activity, history of recent fracture or fall, or laboratory tests, such as those that assess bone turnover, in its calculation. A history of fracture event or fall in a geriatric population implies that the affected individual is more prone to future fracture events than those without such a history.[10] However, to provide a variable that can be compared quantitatively, we calculated FRAX in our patient group. To address its limitation, we additionally analyzed fracture events during the clinical observation period. Any fracture event involving the hip or spine during the observation period or at the start of treatment was recorded. Medical history, history of alcohol consumption, presence of rheumatoid arthritis, and steroid use were recorded. We categorized the patients according to their history of fractures at the time of treatment initiation. The patients were further classified into 3 groups according to the length of denosumab use (in months): 12, 24, and ≥36 months. Finally, we analyzed the effect of denosumab use on BMD and future fracture risk among those who did not receive prior treatment (N=123).
Statistical analysis
For the initial comparison, we calculated the mean BMD value of the entire patient group during each follow-up period and compared the values. Using other variables, a linear mixed model was used to calibrate gradual changes in BMD. In addition, we compared the mean BMD values of the subgroups based on the length of clinical observation using the student’s t-test. The FRAX scores of the subgroups were also compared using the student’s t-test. The incidence of fracture events during follow-up was recorded. Statistical analysis was conducted using SPSS software (SPSS Inc., Chicago, IL, USA).
RESULTS
The patients’ demographic data are presented in Tables 1 and 2. The patient population comprised more women (N=138) than men (N=17). Nine patients (5.8%) experienced additional fracture events during the observation period. In total, 123 patients had no history of osteoporosis treatment. Twenty-two patients (14.1%) were treated with oral or intravenous bisphosphonate. Five patients (3.2%) received recombinant parathyroid hormone, 2 patients (1.3%) received a selective estrogen receptor modulator, romosozumab, and 2 patient (1.3%) received an unknown agent.
According to the length of denosumab use, 51, 47, and 57 patients belonged to the 12, 24, and ≥36 months groups, respectively. In the entire patient group, there was an increase in BMD after the start of treatment (P<0.001) (Fig. 1). A significant increase in BMD (Fig. 2) was also observed during the treatment period. In the 12 months group, lumbar spine BMD increased from −3.04 to −2.57 (P<0.001), femoral neck BMD increased from −3.12 to −2.88 (P=0.003), and total hip BMD increased from −2.47 to −2.16 (P=0.001). In the 24 months group, lumbar spine BMD increased from −2.98 to −2.32 (P<0.001), femoral neck BMD increased from −3.11 to −2.87 (P=0.004), and total hip BMD increased from −2.43 to −2.42 (P=0.903). A similar increase in BMD was observed in the ≥36 months group; lumbar spine BMD increased from −2.51 to −1.63 (P=0.01), femoral neck BMD increased from −3.20 to −2.69 (P<0.001), and total hip BMD increased from −2.57 to −1.89 (P=0.03).

(A, B) Change in bone mineral density in the total patient group (N=155) and in those who had no previous experience of osteoporosis treatment (N=123). Analysis was performed using a linear mixed model. Sites included the lumbar spine (P=0.000), femoral neck (P=0.000), and total hip (P<0.001).
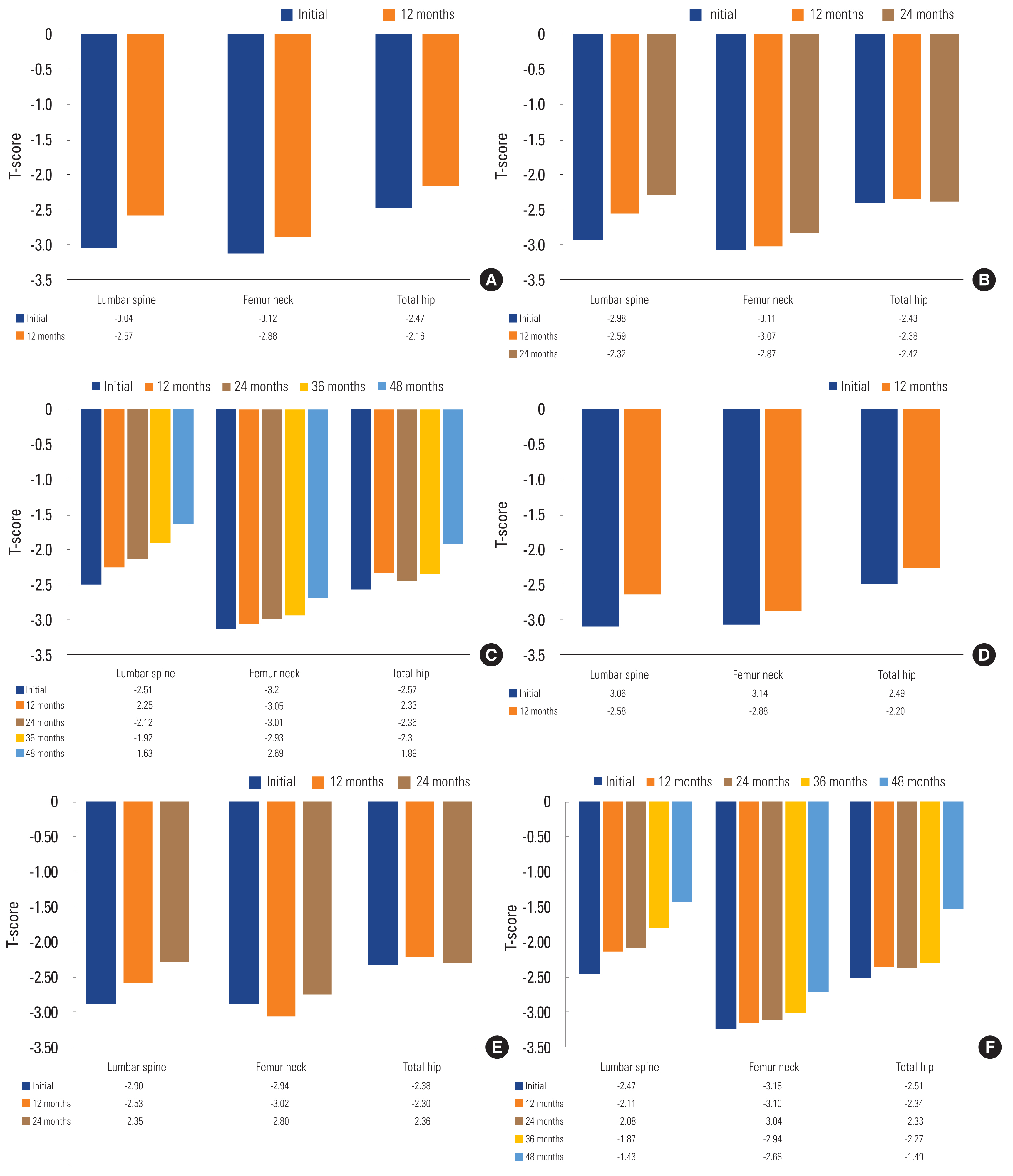
(A–F) Bone mineral density was observed and compared in 6 separate groups. Patients were assigned to each group based on their length of clinical follow-up and their previous experience with osteoporosis treatment
We categorized the data of those with no prior history of osteoporosis treatment (N=123) the same way as the entire data using the length of denosumab use (in months) into 12, 24, and ≥36 months groups. These subgroups had 44, 37, and 42 patients, respectively. BMD significantly increased in the 123 patients. The BMD of the lumbar spine increased from −2.85 to −1.62 (P<0.001), that of the femoral neck increased from −3.11 to −2.68 (P=0.001), and that of the total hip increased from −2.46 to −1.46 (P<0.001). A significant increase in BMD was also observed during the treatment period for all 3 patient subgroups. In the 12 months group, lumbar spine BMD increased from −3.06 to −2.58 (P<0.001), femoral neck BMD increased from −3.14 to −2.88 (P=0.003), and total hip BMD increased from −2.49 to −2.20 (P=0.001). In the 24 months group, lumbar spine BMD increased from −2.90 to −2.35 (P<0.001), femoral neck BMD increased from −2.94 to −2.80 (P=0.146), and total hip BMD increased from −2.38 to −2.36 (P=0.734). A similar increase in BMDs was observed in the ≥36 months group; lumbar spine BMD increased from −2.47 to −1.43 (P=0.004), femoral neck BMD increased from −3.18 to −2.68 (P=0.002), and total hip BMD increased from −2.51 to −1.49 (P=0.03) (Fig. 2).
Reduced FRAX scores were observed in all 3 groups. FRAX scores reduced from 36.71 to 30.65 (P=0.003), 29.27 to 28.40 (P=0.410), and 28.76 to 25.68 (P=0.001) in the 12, 24, and ≥36 months groups, respectively (Fig. 3A). Three patients in the 12 months group (5.9%), 24 months group (6.4%), and ≥36 months group (5.3%) had fracture events (Fig. 4). Of the 155 patients, 9 patients (5.8%) had a fracture event during the clinical observation period, and the occurrence was not significantly different between the subgroups and the total patient cohort (P=0.61). A similar result was found in those with no history of prior treatment. FRAX scores were reduced in all 3 groups. FRAX scores were reduced from 37.42 to 30.88 (P=0.003) in the 12 months group, 31.23 to 30.22 (P=0.43) in the 24 months group, and 30.94 to 28.36 (P=0.002) in the ≥36 months group (Fig. 3B). Three patients in the 12 months group (6.8%), 24 months group (8.1%), and ≥36 months group (7.1%) had a fracture event. Among the 123 patients, 9 patients (7.3%) had a fracture event during the clinical observation period, and the occurrence was not significantly different between the subgroups and the total patient group (P=0.67) (Fig. 4).

(A, B) The fracture risk assessment tool was calculated and compared in each group. Scores decreased in every group with statistically significant decreases in the 12 months and ≥36 months groups (P=0.003, P=0.001). The decrease was not significant in the 24 months group (P=0.410).
DISCUSSION
Osteoporosis is a condition that affects bone turnover rate.[10] Studies have shown that it can be caused by various factors, including decreased sex hormone levels, poor nutritional absorption, and decreased levels of physical exercise.[4] Thus, it can be inferred that the incidence of osteoporosis increases with age, and a population-level study conducted by Ahn et al. [11] in Korea confirmed this trend in 2020. Amongst the clinical implications of osteoporosis, its association with increased fracture risk in older people is particularly important. Patients with osteoporotic bones are more likely to be susceptible to fractures with relatively minor trauma, such as falls, than those with non-osteoporotic bones.[10,12] Since fractures may lead to mortality in elderly patients, osteoporosis treatment is crucial in senile healthcare.[13] In several previous studies, denosumab, an antiresorptive osteoporosis medication that acts as a receptor activator of nuclear factor-κB ligand inhibitor, increased bone mass and reduced fracture risk.[8,14–16] Many years after its release, denosumab is still considered to maintain and increase bone mass when combined with other medications, such as bisphosphonate or teriparatide.[14,17] This increase in bone mass was shown to reduce fracture risk; thus, by using denosumab, physicians can expect a reduction in the risk of osteoporotic fractures.[6,7,10,18] Previous studies have also demonstrated increased bone mass in patients aged >80 years. In their review of 257 patients, Çiğiloğlu et al. [19] reported that the difference in the effect of denosumab on BMD was non-significant between those over 80 and those younger than 80. Our study tested 155 patients within a 36-month follow-up from the initial injection. The same result was found among those who received denosumab for 12 months and those who received it for 24 or 36 months or more. Additionally, a significant difference in FRAX scores was observed between the onset of treatment and the latest bone densitometry. Moreover, the effects of increasing bone mass and lowering fracture risk were observed in those with a history of fracture at the time of denosumab treatment initiation and those without. Additionally, the efficacy of denosumab was shown in those with no history of osteoporosis treatment.
Only a few studies in Korea with a sample of more than 60 patients aged 80 and above have reviewed the ability of denosumab to increase BMD and lower the possibility of further fracture events. From this perspective, our study supports the efficacy of denosumab, regardless of patient age, in preventing osteoporosis. However, this study has several limitations. Bone turnover markers were not measured in our patients during the clinical observation. A lack of this monitoring of metabolic activity is not ideal as increased bone turnover is a characteristic of senile patients with osteoporosis, as reported in patients who discontinued their treatment and experienced increased bone turnover.[20–22] However, the increase in BMD and the lower incidence of further fracture events after denosumab administration supports our hypothesis. Furthermore, the FRAX alone is considered an inadequate metric in clinical practice owing to its many limitations, such as its limited reflection of BMD, the presence of a fall, or any other low-energy trauma, among others.[9] However, our study also investigated the incidence of other fracture events during the clinical observation period. Finally, during our analysis, the effect of denosumab in reducing FRAX scores and increasing BMD showed insignificant changes, although the result shows an improvement. This was shown in the total patient group and those with no history of osteoporosis treatment. Since these groups had no differences in demographic data except for the length of denosumab use, the cause remains obscure. This would need further assessment, and more clinical data obtained by observation might be required.
Managing osteoporosis is important, considering the aging curve and its rate of change in the Korean population. Treating and regularly measuring bone density may decrease the risk of future fractures, especially in the hip, spine, and wrist. Among these agents, denosumab is a favorable option for treating osteoporosis and preventing further fracture events in the senile population, especially in those aged over 80 years.
Notes
Ethics approval and consent to participate
The study protocol conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki and was approved by the Institutional Review Board of Dankook University Hospital.
Conflict of interest
No potential conflict of interest relevant to this article was reported.