 |
 |
| jbm > Volume 30(1); 2023 > Article |
|
Abstract
Background
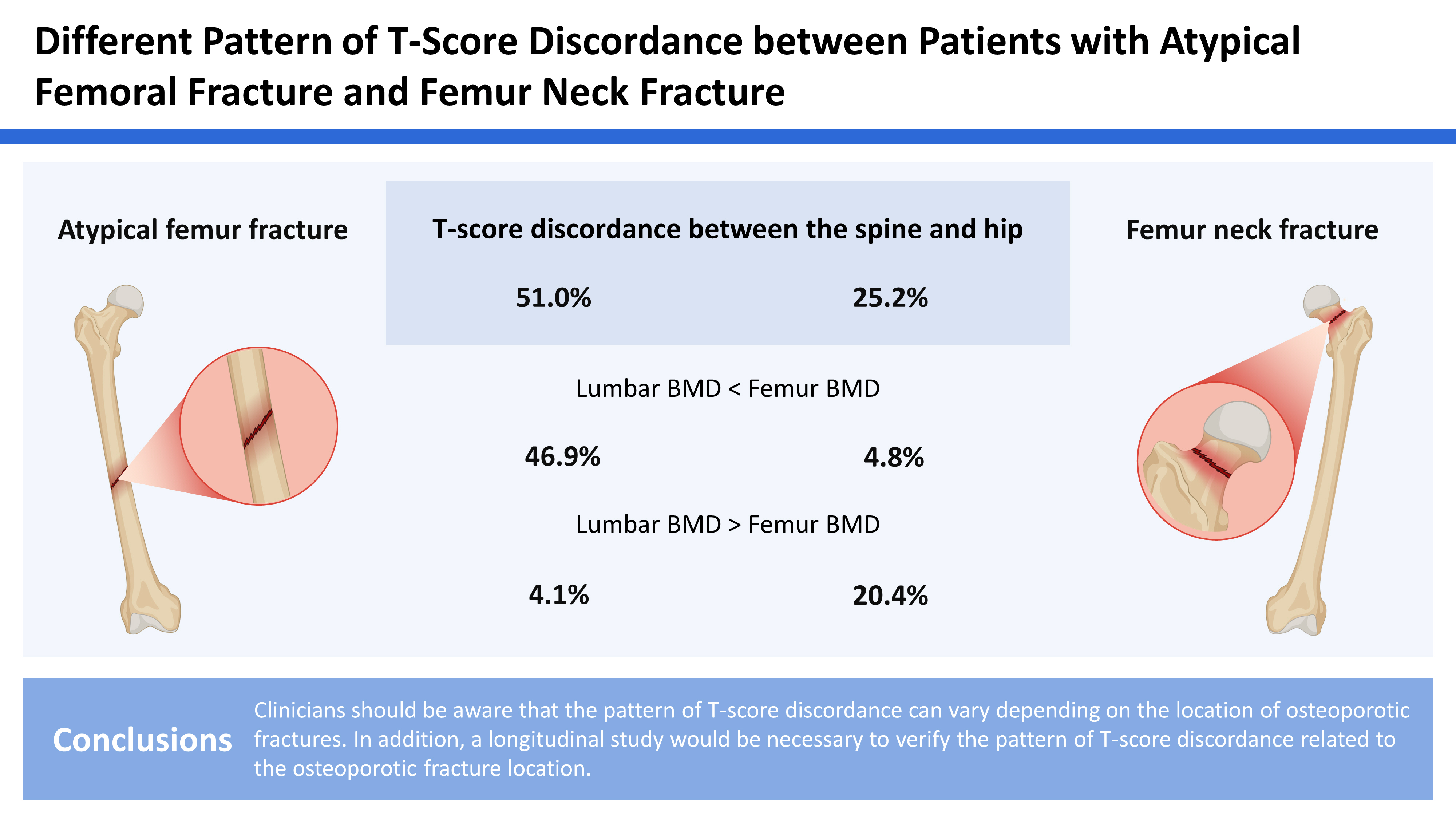
Our study evaluated the prevalence and pattern of T-score discordance between the spine and hip in Korean patients with atypical femoral fracture (AFF) and femur neck fracture (FNF).
Methods
A total of 49 patients (all women) who were treated for AFF and 1:3 matched 147 female patients with FNF were included from January 2012 to August 2022. A discordance of more than 1.5 between lumbar spine and femur neck bone mineral density (BMD) was defined as a difference and divided into 3 groups: lumbar low (LL; lumbar BMD is less than femur neck BMD), no discordance (ND), and femur neck low (FL; femur neck BMD is less than lumbar BMD). We compared the prevalence and pattern of discordance between 2 groups, and the associated risk factors of T-score discordance among the subjects were evaluated using regression analysis.
Results
The prevalence of discordance was significantly higher in patients with AFF (51%) than in those with FNF (25.2%; P<0.001). LL discordance was found in 46.9% of the patients with AFF but only 4.8% in those with FNF. Conversely, FL discordance was found in 4.1% of the patients with AFF and 20.4% in those with FNF, respectively. No specific risk factor was found as T-score discordance in the 2 groups.
Osteoporotic hip fractures in the elderly usually need surgical treatment to decrease morbidity and mortality.[1] Also, it is essential to manage osteoporosis after surgery of hip fracture to prevent a second osteoporotic fracture and dual energy X-ray absorptiometry (DXA) is a standard tool to evaluate bone mineral density (BMD).[2] However, clinicians commonly observe the discordance in T-score at the 2 different skeletal sites (lumbar spine and hip) known to increase fracture risk.[3,4] Spine-hip discordance (SHD) can be categorized into lumbar low (LL) discordance (lumbar BMD is lower than femur neck BMD), no discordance (ND) and femur neck low (FL) discordance (femur neck BMD is lower than lumbar BMD).[5,6]
Recently, several studies investigated the prevalence and impact of SHD on the management of osteoporosis. One comparative study revealed that the prevalence of LL discordance was significantly higher in atypical femoral fractures (AFF) patients than in the Korean osteoporosis population (63.5% vs. 31.7%).[7] Another study also has shown that patients with AFF have a significantly higher prevalence of LL discordance than elderly patients who were treated with intertrochanteric fractures.[8] However, a large cohort study of 1,090 fragility hip fractures showed higher rates of FL discordance compared to the general population.[9] Thus it seems to be there are differences in pattern of discordance according to the fracture site or type.[10]
Studies on the prevalence and factors of T-score discordance in Korea are still lacking, and no studies have examined discordance of AFFs when compared with patients who were treated with osteoporotic femur neck fracture (FNF). The aim of current study is to compare the prevalence and risk factors of SHD between patients with AFF and FNF from a single tertiary orthopedic institution.
We carried out a retrospective review of patients diagnosed with femur shaft and sub-trochanter fractures under the official approval of the Institutional Review Board (EUMC 2022-10-020). From January 2012 to August 2021, we identified 292 patients treated with femur shaft or sub-trochanter fractures. We excluded patients treated with comminuted fracture (N=211) or supra-condylar femoral fracture (N=7).
AFF was defined as met at least 4 of the 5 major criteria of 2014 The American Society for Bone and Mineral Research definition.[11,12] The AFF was properly treated based on current treatment principles with intramedullary nailing. After reviewing X-ray, 8 patients who had pathologic (metastatic) fractures and 11 patients without DXA were excluded, and 49 patients were finalized.
There were 40 femur shaft fractures (81.6%), 9 femur subtrochanteric fractures (18.4%). All were female and 46 patients (93.9%) had been treated with osteoporosis treatment. The average age at the time of fracture was 76.9 years (range, 61-92 years) and other demographic data are presented in Table 1.
The comparative group was selected from the pool of patients from 630 consecutive patients who had been treated with FNF. Confounding factors included age, sex, body mass index (BMI) and Charlson Comorbidity Index (CCI). Based on these variables, 1:3 propensity score matching patient match was done using propensity scores estimated on the scale of the log odds under a logistic regression mode.
Bone density measurements were performed on the proximal femur proximal part of the femur (neck and total hip) and lumbar spine using a Lunar Prodigy scanner (Lunar Corp., Madison, WI, USA) Mean lumbar spine areal BMD values were used from at least 2 evaluable vertebrae from L1 to L4, and if there was a focal structural defect or a discrepancy of >1 standard deviation (SD) in T-score between adjacent vertebrae, the physicians excluded that vertebral level. The femoral neck and total hip T-scores were measured in unfractured femur, and the lowest score at either site was used as the femoral T-score for the analysis. All densitometry was performed within 1 month after fracture occurrence. The difference in the discordance between L1-4 and femur neck BMD was defined as ≥1.5 SD, and was divided into 3 groups: LL, ND, and FL groups.[13]
We evaluated the prevalence and compared the type of T-score discordance between patients with AFFs and FNFs. To determine associated risk factors for T-score discordance, we first investigated demographic differences between the concordance and discordance groups and assessed medical conditions affecting osteoporosis including age, BMI, BMD, CCI, and previous history of osteoporotic treatment.
According to the normal distribution, Student’s t-tests or Mann-Whitney U test was used to compare continuous data, and the χ2 test or Fisher’s exact test was used to analyze categorical data. For all other tests, a 2-sided P-value of 0.05 was considered significant. To determine the risk factors of discordance, multivariable regression analysis was performed in variables with a P-value less than 0.1. Statistical analyses were conducted with the SPSS for Windows statistical package, version 16.0 (SPSS Inc., Chicago, IL, USA). The level of significance was set at P less than 0.05.
According to the World Health Organization classification, there were 41 patients (83.7%) with osteoporosis, 6 (12.2%) with osteopenia, and 1 (2%) with a T-score in the normal range in the AFF patients. In all cases, T-score discordance found in 25 out of 49 cases was 51%. Among them, there was a LL discordance in 23 cases (46.9%), and 2 patients (4.1%) had FL discordance.
The prevalence of osteoporosis among 147 FNF patients were 81.0% (119 patients) and other 28 patients were diagnosed with osteopenia. Discordance was found in 37 patients (25.2%) with FNF, so significantly lower than those with AFF (P<0.001). Among them, there was a LL discordance in 7 cases (4.8%), and 30 patients (20.4%) had low FN discordance (Table 1).
Previous history of osteoporosis treatment, weight, height, BMI, and CCI did not differ between the concordance and discordance groups (Table 2). However, BMD T-score did differ significantly between these groups. Multivariable analysis was not able due to statistical significance.
Our study shows that the pattern of T-score discordance is obviously different according to the hip fracture type even co-variants including their age were matched. The incidences and patterns of SHD are known to be different according to their age.[14-16] Because different bone turnover rate of cortical and cancellous bones plays a major role in SHD in middle-aged women, but various degenerative changes such as osteoarthritic spurs, and calcification of aorta are associated in older age (>70 years).[6,17,18]
SHD is an upcoming issue because it is known to increase osteoporotic fracture risk. One previous study of 1,090 hip fractures showed ND itself, but the FL discordance type may be a strong risk factor for hip fracture which needs further treatment.[9] Otherwise, our previous study showed that LS discordance was main pattern (81.3%) in patients with an osteoporotic vertebral compression fracture.[10] It is notable because T-score of the spine is usually higher than that of the hip in the elderly over 70 years of age due to degenerative changes.[15,19] Considering the above results, clinicians need to know the possibility of discordance and type to predict osteoporotic fracture.[20]
We usually follow-up BMD using DXA, but only BMD not discordance was considered to predict major osteoporotic fracture. Only T-score was focused, but the combination of these 2 skeletal regions (lumbar spine and femur) also be an important factor when we follow up with patients.[21] It might be the improvement of BMD is not the same between the anatomic regions as the rates of bone loss also differ substantially in the same individual.[22]
From multicenter prospective study revealed that higher BMI and use of bisphosphonate were significant risk factors of AFF.[23] The development of atypical fractures is not associated with osteoporosis but pathophysiology of stress fracture due to altered bone structure and biomechanics.[24] It has been proposed that patients with long-term use of bisphosphonate may have a low bone turnover condition with impaired new bone formation and our patients with AFF are also mostly treated with anti-resorptive (93.9%, 46 of 49). In this context, we feel that clinicians should notice whether the pattern of improvement will go discordance or not to predict AFF.
The incidence of SHD was relatively low compared to similar Korean studies (Table 3). Two criteria for discordance are now used and cited in recent studies (1) a discrepancy in the BMD measurements at the 2 sites; (2) a difference between L1-4 and femur neck BMD more than 1.5 SD.[8,25-28] However, it might not be related to physiologic change or the increased risk of fracture if discordance was diagnosed with a lumbar T-score of −2.4 and femur neck of −2.5. Thus, we selected the criteria of difference >1.5 SD and general criteria of discordance also need to be established.
The present study has some limitations. First, the design of our study was retrospective and included a number of patients that were relatively small. Second, we could not evaluate potential risk factors including the age of menopause or the type of osteoporosis treatment because many of our patients were too old to remember exact age.
Considering the interest in SHD, clinicians need to be aware that the pattern of T-score discordance can vary depending on the location of osteoporotic fractures. Also, a longitudinal study would be necessary to verify the pattern of T-score discordance is really related to the osteoporotic fracture location.
DECLARATIONS
Table 1
Clinical details of included patients
Table 2
Comparison of clinical values in patients who had been treated with atypical femoral fracture and femur neck fracture
Table 3
Prevalence of T-score spine-hip discordance form previous Korean studies
| References | Year | Enrollment period | Included fracture type | N | FL | LL | ND | Mean age at Fx (yr) |
|---|---|---|---|---|---|---|---|---|
| Yoon et al. [10] | 2022 | 2015-2021 | Osteoporotic vertebral compression fractures | 200 | 11 (5.5) | 52 (26.0) | 137 (68.5) | 81.3 |
| Lee et al. [9] | 2022 | 2011-2020 | Osteoporotic hip fractures | 1,090 | 243 (22.3) | 44 (4.0) | 803 (73.7) | 78.5 |
| Choi et al. [7] | 2022 | 2010-2021 | Atypical femoral fracture | 63 | 4 (6.3) | 40 (63.5) | 19 (30.2) | 73.7 |
| Lee et al. [8] | 2017 | 2009-2016 | Atypical femoral fracture/ Osteoporotic intertrochanteric fracture | 48/114 | 3 (6.3)/− | 31 (64.6)/− | 14 (29.2)/ 88 (77.2) | 73.0 |
| Current study | 2023 | 2012-2021 | Atypical femoral fracture/ Osteoporotic femur neck fracture | 49/147 | 2 (4.1)/ 30 (20.4) | 23 (46.9)/ 7 (4.8) | 24 (49.0)/ 110 (74.8) | 76.9 |
REFERENCES
1. Chukir T, Haseltine K, Do H, et al. Clinical characteristics and fracture patterns among postmenopausal women with isolated osteoporosis at the forearm. J Clin Densitom 2022;25:208-14. https://doi.org/10.1016/j.jocd.2021.07.012.


2. Masud T, Giannini S. Preventing osteoporotic fractures with bisphosphonates: a review of the efficacy and tolerability. Aging Clin Exp Res 2003;15:89-98. https://doi.org/10.1007/bf03324485.


3. Glüer CC. 30years of DXA technology innovations. Bone 2017;104:7-12. https://doi.org/10.1016/j.bone.2017.05.020.


4. Larcos G. Predicting clinical discordance of bone mineral density. Mayo Clin Proc 1998;73:824-8. https://doi.org/10.4065/73.9.824.


5. El Maghraoui A, Mouinga Abayi DA, Ghozlani I, et al. Prevalence and risk factors of discordance in diagnosis of osteoporosis using spine and hip bone densitometry. Ann Rheum Dis 2007;66:271-2. https://doi.org/10.1136/ard.2006.062372.



6. Moayyeri A, Soltani A, Tabari NK, et al. Discordance in diagnosis of osteoporosis using spine and hip bone densitometry. BMC Endocr Disord 2005;5:3.https://doi.org/10.1186/1472-6823-5-3.



7. Choi YS, Kim TW, Jeong JH, et al. Comparative analysis of T-score discordance between a registry-based Korean population and atypical femoral fracture patients of a single institution. Clin Orthop Surg 2022;14:352-60. https://doi.org/10.4055/cios21258.



8. Lee KJ, Min BW, Song KS, et al. T-score discordance of bone mineral density in patients with atypical femoral fracture. J Bone Joint Surg Am 2017;99:1683-8. https://doi.org/10.2106/jbjs.16.01440.


9. Lee KH, Park JW, Kim S, et al. Prevalence, clinical implication, and cause of spine hip discordance in elderly patients with fragility hip fracture. J Bone Metab 2022;29:51-7. https://doi.org/10.11005/jbm.2022.29.1.51.



10. Yoon BH, Kang HW, Kim SM, et al. Prevalence and risk factors of T-score spine-hip discordance in patients with osteoporotic vertebral compression fracture. J Bone Metab 2022;29:43-9. https://doi.org/10.11005/jbm.2022.29.1.43.



11. Alexandru D, So W. Evaluation and management of vertebral compression fractures. Perm J 2012;16:46-51. https://doi.org/10.7812/tpp/12-037.



12. Diacinti D, Guglielmi G. How to define an osteoporotic vertebral fracture? Quant Imaging Med Surg 2019;9:1485-94. https://doi.org/10.21037/qims.2019.09.10.



13. Woodson G. Dual X-ray absorptiometry T-score concordance and discordance between the hip and spine measurement sites. J Clin Densitom 2000;3:319-24. https://doi.org/10.1385/jcd:3:4:319.


14. Yoon BH, Kim DY. Discordance between hip and spine bone mineral density: A point of care. J Bone Metab 2021;28:249-51. https://doi.org/10.11005/jbm.2021.28.4.249.


15. Leslie WD, Lix LM, Johansson H, et al. Spine-hip discordance and fracture risk assessment: a physician-friendly FRAX enhancement. Osteoporos Int 2011;22:839-47. https://doi.org/10.1007/s00198-010-1461-5.


16. McMahon K, Kalnins S, Freund J, et al. Discordance in lumbar spine T-scores and nonstandardization of standard deviations. J Clin Densitom 2003;6:1-6. https://doi.org/10.1385/jcd:6:1:1.


17. Nugent SD, Kaats GR, Preuss HG. Discordance between body mass index (BMI) and a novel body composition change index (BCCI) as outcome measures in weight change interventions. J Am Coll Nutr 2018;37:302-7. https://doi.org/10.1080/07315724.2017.1397566.


18. McMahon K, Nightingale J, Pocock N. Discordance in DXA male reference ranges. J Clin Densitom 2004;7:121-6. https://doi.org/10.1385/jcd:7:2:121.


19. Hong AR, Kim JH, Lee JH, et al. Metabolic characteristics of subjects with spine-femur bone mineral density discordances: the Korean National Health and Nutrition Examination Survey (KNHANES 2008-2011). J Bone Miner Metab 2019;37:835-43. https://doi.org/10.1007/s00774-018-0980-6.


20. Alarkawi D, Bliuc D, Nguyen TV, et al. Contribution of lumbar spine BMD to fracture risk in individuals with T-score discordance. J Bone Miner Res 2016;31:274-80. https://doi.org/10.1002/jbmr.2611.


21. Younes M, Ben Hammouda S, Jguirim M, et al. Discordance between spine and hip bone mineral density measurement using DXA in osteoporosis diagnosis: Prevalence and risk factors. Tunis Med 2014;92:1-5.

22. Abrahamsen B, Stilgren LS, Hermann AP, et al. Discordance between changes in bone mineral density measured at different skeletal sites in perimenopausal women--implications for assessment of bone loss and response to therapy: The Danish Osteoporosis Prevention Study. J Bone Miner Res 2001;16:1212-9. https://doi.org/10.1359/jbmr.2001.16.7.1212.


23. Lee YK, Kim TY, Ha YC, et al. Atypical subtrochanteric fractures in Korean hip fracture study. Osteoporos Int 2017;28:2853-8. https://doi.org/10.1007/s00198-017-4112-2.


24. Larsen MS, Schmal H. The enigma of atypical femoral fractures: A summary of current knowledge. EFORT Open Rev 2018;3:494-500. https://doi.org/10.1302/2058-5241.3.170070.



25. Goh TS, Kim E, Jeon YK, et al. Spine-Hip Discordance and FRAX assessment Fracture Risk in Postmenopausal Women with Osteopenia from Concordant Diagnosis Between Lumbar Spine and Femoral Neck. J Clin Densitom 2021;24:548-56. https://doi.org/10.1016/j.jocd.2021.03.008.

26. Leslie WD, Morin SN, Lix LM, et al. Impact of spine-hip discordance on fracture risk assessment and treatment qualification in Canada: the Manitoba BMD registry. Arch Osteoporos 2020;15:85.https://doi.org/10.1007/s11657-020-00763-y.


27. Chan CY, Subramaniam S, Mohamed N, et al. Prevalence and factors of T-score discordance between hip and spine among middle-aged and elderly Malaysians. Arch Osteoporos 2020;15:142.https://doi.org/10.1007/s11657-020-00821-5.


28. Seok H, Kim KJ, Kim KM, et al. High prevalence of spine-femur bone mineral density discordance and comparison of vertebral fracture risk assessment using femoral neck and lumbar spine bone density in Korean patients. J Bone Miner Metab 2014;32:405-10. https://doi.org/10.1007/s00774-013-0512-3.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,553 View
- 53 Download
- ORCID iDs
-
Byung-Ho Yoon

https://orcid.org/0000-0001-8518-6331Jang-Won Park

https://orcid.org/0000-0001-6269-6451Chan Woo Lee

https://orcid.org/0000-0003-2215-2171Young Do Koh

https://orcid.org/0000-0002-3784-7059 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



