 |
 |
| jbm > Volume 29(3); 2022 > Article |
|
Abstract
Ectopic parathyroid adenomas of the retropharyngeal space are relatively rare. Herein, we report a case of primary hyperparathyroidism (PHPT) secondary to a retropharyngeal parathyroid adenoma. A 22-year-old woman presented with elevated serum calcium and parathyroid hormone (PTH) levels, revealed during a medical check-up. The patient had a history of ureteral stones and a confirmed low bone mass. Neck 99mTechnetium-sestamibi singlephoton emission computed tomography (CT) and ultrasonography did not reveal any suspicious lesions. There was no evidence of hereditary PHPT based on the results of targeted gene sequencing. Surgical exploration was unsuccessful, and the PHPT persisted after the first surgery. Approximately a year after the failed operation, 18F-fluorocholine (FCH) positron emission tomography/CT (PET-CT) became available, and when performed, it revealed increased uptake in the retropharyngeal space of the right side of the neck. The results of parathyroid venous sampling were concordant with a >2-fold elevation of PTH level in the veins on the right side of the neck compared to the peripheral veins. The 1.8 cm-diameter mass was successfully removed resulting in an 87% reduction in intraoperative PTH level (198.0-26.5 pg/mL). Subsequently, normalizations of calcium and PTH levels were achieved. In summary, ectopic parathyroid adenomas, including retropharyngeal lesions, should also be suspected when investigating an elusive case of PHPT. 18F-FCH PET-CT can be a useful complementary modality for detecting culprit lesions.
Primary hyperparathyroidism (PHPT) is a pathological condition in which one or more parathyroid glands produce excessive levels of parathyroid hormone (PTH). A total of 89% of PHPT cases are caused by a single parathyroid adenoma, and localization of the parathyroid adenoma is essential for curative treatment.[1] Parathyroid adenomas typically arise immediately posterior or inferior to the thyroid gland in 80% to 85% of patients with PHPT.[2] In contrast, ectopic parathyroid adenomas, located elsewhere than the thyroid, occur in 15% to 20% of these patients, with the anterior mediastinum being the most common location.[2] However, the retropharyngeal region has rarely been reported as a location of parathyroid adenomas.[2]
PHPT is diagnosed based on hypercalcemia and elevated PTH levels.[1] Once PHPT is confirmed, imaging modalities such as ultrasonography and 99mTechnetium sestamibi imaging (sestamibi scan) with or without singlephoton emission computed tomography (SPECT) are usually used as a first-line modality for localization of the parathyroid adenoma.[3] Despite the high sensitivity and positive predictive value (PPV) of first-line modalities, localization studies of ectopically located parathyroid adenomas could fail. When first-line imaging studies provide insufficient evidence, surgical exploration is the option for patients with PHPT.[3] However, even with various imaging modalities, 38.3% (N=836) of 2,185 PHPT patients failed to localize the adenoma.[3] Therefore, other imaging methods are used in the research protocol to locate parathyroid adenomas more precisely.[4] For instance, a case presented by Iconaru et al. [5] reported that 18F-fluorocholine (FCH) positron emission tomography/computed tomography (PET-CT) was useful in localizing an ectopic parathyroid adenoma in the retropharyngeal space, which is a very unusual and elusive location even in ectopic cases.
In this report, we present the case of a 22-year-old woman with PHPT and an ectopic retropharyngeal parathyroid adenoma located on FCH PET-CT.
A 22-year-old woman was referred to our hospital in April 2019 because of elevated calcium and PTH levels found during a medical check-up. The patient had a history of urolithiasis 4 years ago but no history of fractures, PHPT, or other endocrinopathies. The patient’s family history included an aunt who had undergone surgery for thyroid cancer. The patient had no specific acute hypercalcemic symptoms, and her physical examination was unremarkable.
In the initial laboratory tests, the patient showed elevated serum calcium (11.4 mg/dL, normal 8.5-10.5 mg/dL) and PTH (256.5 pg/mL, normal 15-65 pg/mL) levels with low serum phosphorus (1.7 mg/dL, normal 2.8-4.5 mg/dL) levels, consistent with PHPT. Bone turnover markers such as serum C-terminal telopeptide of type I collagen (CTX) and osteocalcin were elevated (CTX 1.060 ng/mL, normal ≤0.573 ng/mL; osteocalcin 47.80 ng/mL, normal 11-43 ng/mL). Her 24-hr urine calcium level was also high at 297 mg/24 hr. The patient’s Z-score was −3.2 at the lumbar spine, −2.9 at the femur neck, and −2.3 at the total hip, and low bone mass was confirmed.
Based on the patient’s young age and family history of thyroid cancer, additional studies were conducted to rule out familial diseases such as multiple endocrine neoplasia type 1 (MEN1). A pituitary microadenoma on the left lateral wing on brain magnetic resonance imaging is most likely a benign non-functioning tumor considering her normal blood pituitary hormone levels. No other abnormalities were found on endoscopic ultrasonography of the pancreas or Ga-68 DOTATOC PET-CT. MEN1 was finally ruled out using next-generation sequencing results.
Primary localization studies for PHPT followed, including a sestamibi scan with SPECT and neck ultrasonography, but showed no remarkable lesion suggestive of parathyroid adenoma. There was no further available imaging modality, such as FCH PET-CT; therefore, parathyroid venous sampling (PVS) was performed.[6] It revealed a 2-fold PTH elevation at the bifurcation site of the right subclavian vein and internal jugular vein, suggesting that the adenoma was located on the right side (Fig. 1).
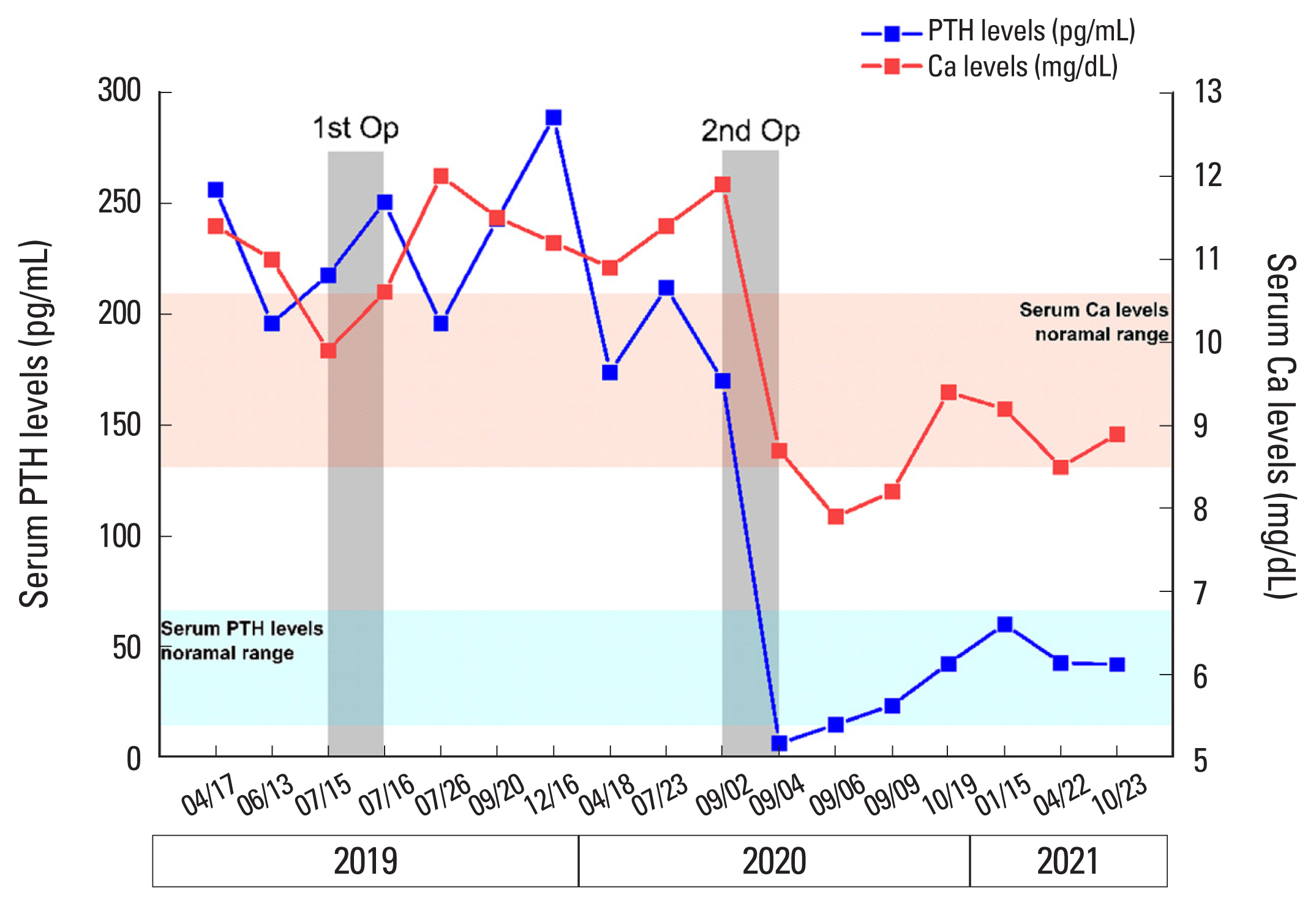
The patient underwent surgical exploration 2 months after her initial visit based on the PVS results. The right inferior, right superior, and left inferior parathyroid glands were removed sequentially; however, there was an insignificant change in intraoperative PTH levels, dropping from 288 pg/mL to 213.3 pg/mL (26% reduction). Upon suspicion of an ectopic parathyroid gland, a complete thymectomy was performed, but there was no change in intraoperative PTH levels. Therefore, the patient was followed-up with consistent medical treatment for persistent hyperparathyroidism. Further localization studies were planned to identify the remnant ectopic parathyroid tumors.
A month later, C-11 methionine (MET) PET-CT was performed, but the result was negative. After one year of follow-up, FCH PET-CT was newly introduced in our institution in 2020, and the patient was re-evaluated using this up-to-date modality. Finally, there was increased uptake at right neck level II, concordant with previous PVS findings (Fig. 2).
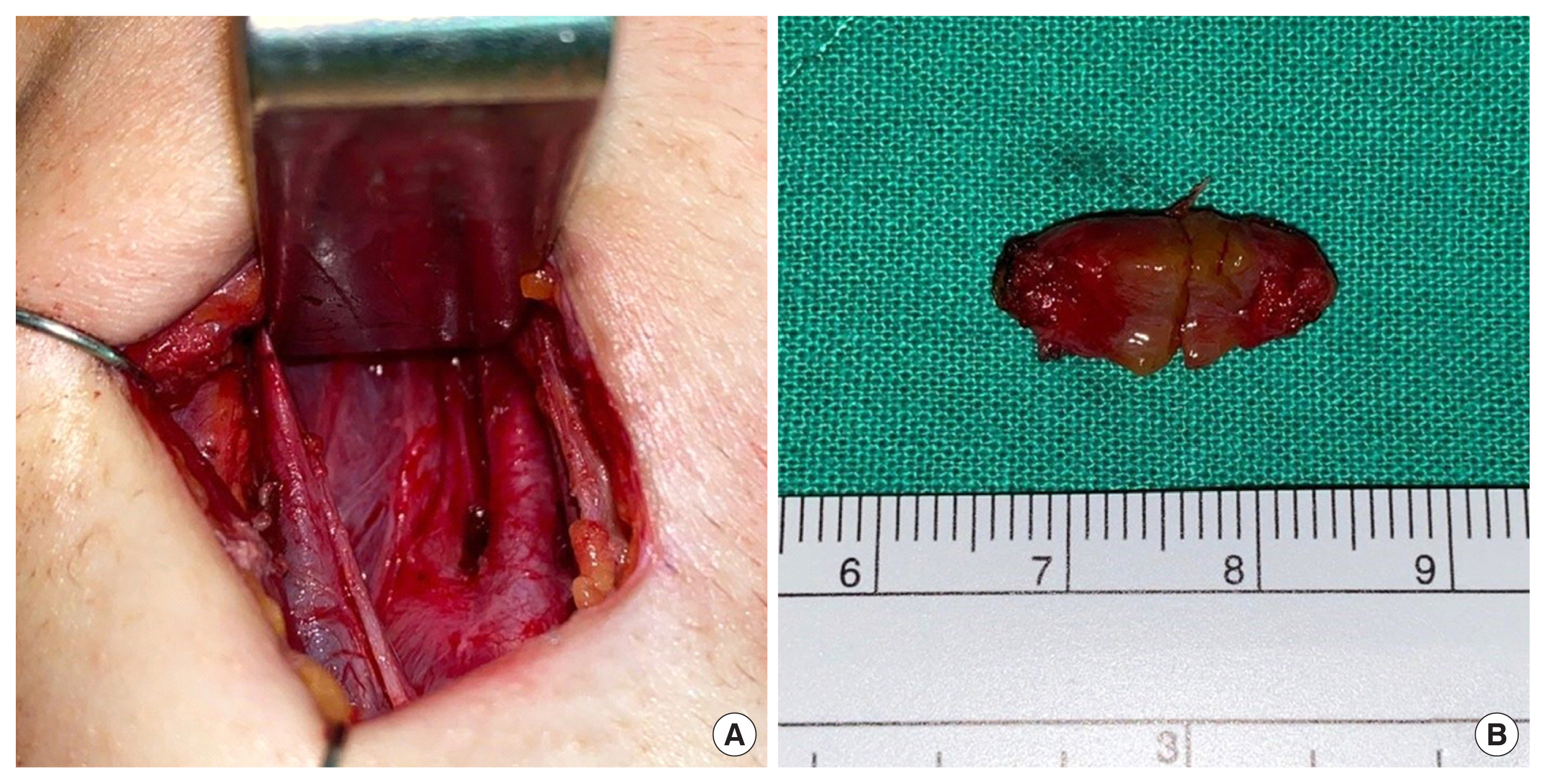
Therefore, a second surgery was performed 14 months after the first surgery. An abnormally colored level II lymph node in the right neck was identified and excised. However, the change in PTH levels (198 pg/mL) measured by the intraoperative rapid PTH assay was inconclusive. Upon further exploration, a 1.8 cm-sized parathyroid-like tissue was found in the retropharyngeal space, posterior to the right internal jugular vein and 1 cm above the common carotid artery bifurcation (Fig. 3). Pathology confirmed a 1.0×0.8 ×0.3-cm parathyroid adenoma. After excision, the PTH level dropped to 26.5 pg/mL with an 87% reduction of intraoperative PTH (198.0-26.5 pg/mL).
After discharge, the serum PTH and calcium levels normalized successfully and were followed up stably (Fig. 4). The patient presented with hoarseness and temporarily decreased vocal cord mobility after surgery, but vocal cord mobility recovered 10 months later. Seven months after the second surgery, bone density improved (Z-score at the lumbar spine, −1.8; femur neck, −2.8; total hip, −1.8).
Ectopic parathyroid adenomas need to be considered in patients with PHPT who have either yet to localize their adenoma or have had unsuccessful initial surgery. In unexplored patients with PHPT, the prevalence of ectopic parathyroid adenoma was 17.5% to 22%.[7] On the other hand, in patients undergoing reoperation due to missed adenomas, the prevalence of ectopic parathyroid adenoma is 66%.[8]
There is a wide range of possible sites, as ectopic parathyroid glands may be located anywhere along the migratory path during parathyroid organogenesis. The inferior parathyroid gland develops from the third pharyngeal pouch to the thyroid gland, while the superior parathyroid gland develops in the thymus from the fourth pharyngeal pouch. Ectopic parathyroid adenomas occur because of incomplete or variant migration during development.[2] Ectopic parathyroid glands can develop anywhere from the base of the tongue to the mediastinum. Ectopic inferior parathyroids occur intraoperatively (approximately 30%), in the anterosuperior mediastinum (22%), intrathyroidal (15%-22%), and within the thyrothymic ligament (17%). Ectopic superior parathyroids occur in the tracheoesophageal groove (43%), retroesophageal (22%), and posterosuperior mediastinum (14%).[2]
Retropharyngeal ectopic parathyroid adenomas are uncommon among ectopic parathyroid adenomas. Shin et al. [9] reported that among 220 parathyroid specimens excised from 173 re-operative patients, 84 (38.2%) were ectopic parathyroid specimens. Only 6 retropharyngeal ectopic parathyroid specimens (7%) were found in the re-operative patients in this study. Furthermore, Gallagher et al. [10] reported that retropharyngeal ectopic parathyroid adenomas accounted for 47 (1.6%) of 3,006 patients who underwent surgery for sporadic PHPT. Ten (21.3%) of the patients with retropharyngeal ectopic parathyroid adenoma had unremarkable preoperative imaging findings, and 26 were found only after exploring typical anatomic and other common ectopic locations. During the initial surgery, retropharyngeal ectopic parathyroid adenomas were found in only 1.4% (39/2,861) of patients. In contrast, there was a 4-fold increase in the discovery rate at reoperation to 5.5% (8/145).[10]
This is the first case report of retropharyngeal ectopic parathyroid adenoma in Korea and emphasizes the potential of a retropharyngeal mass when ectopic parathyroid adenoma is suspected. Thus, in persistent PHPT despite parathyroid surgery, a systemic approach is needed to locate the ectopic parathyroid glands, including a modality to explore the retropharyngeal space. Although rare, retropharyngeal adenomas should be considered in patients with suspected ectopic parathyroid adenoma, especially if primary imaging modalities and initial surgery have failed to detect the culprit lesion.
Many modalities are used for the localization of parathyroid adenomas. Sestamibi scan, FCH PET-CT, and MET PET-CT are typical CT-based modalities. Sestamibi scan is the most widely performed first-line imaging modality with ultrasonography because of its high sensitivity and wide availability.[7] However, in patients with retropharyngeal parathyroid adenoma or multinodular goiters, lesions could be missed in the sestamibi scan.[10]
FCH PET-CT is a recently proposed modality for localization of parathyroid adenomas, and the research protocol is in progress, expecting FCH PET-CT to perform a substantial role in elusive cases.[11,12] Several studies have reported that the sensitivity and PPV of localization using FCH are better than existing first-line modalities. The sensitivity and PPV of neck ultrasonography were reported to be 76.1% and 93.2%, respectively, and the sensitivity and PPV of sestamibi scan were 78.9% and 90.7%, respectively, whereas Uslu-Beşli et al. [13] reported that the sensitivity and PPV of FCH PET-CT were 94.1% and 97.9%, respectively. FCH PET-CT showed better performance than the first-line localization methods.
Furthermore, FCH PET-CT may be useful for localizing small or ectopic parathyroid adenomas, which are not found in conventional modalities.[14] According to the clinical trial of Thanseer et al. [15], FCH PET/CT had superior sensitivity to sestamibi scan and ultrasonography (100% vs. 66.6% and 16.7%, respectively) in 6 patients with ectopic parathyroid adenomas. Consistent with these studies, in this case, FCH PET-CT revealed a retropharyngeal parathyroid adenoma at a unique location among unlocalized ectopic parathyroid adenomas.
MET PET-CT could be used for the detection of lesions in unlocalizable PHPT.[16,17] MET PET-CT has low thyroidal tracer uptake and is superior to conventional imaging in detecting parathyroid adenomas, including ectopic parathyroid adenomas.[17,18] However, in this case, MET PET-CT failed to find ectopic parathyroid adenoma while FCH PET-CT succeeded in detecting the lesions. Bioletto et al. [19] report that FCH PET-CT has higher sensitivity than MET PET-CT and a similar PPV (92% vs. 80%, 94% vs. 95%, respectively) in parathyroid adenomas, and there is a report that FCH PET-CT was advantageous in detecting small parathyroid adenomas.[14] These studies support why FCH PET-CT was more helpful in finding a small ectopic parathyroid adenoma in this case, although there are limited studies directly comparing the performance of FCH PET-CT and MET PET-CT in ectopic parathyroid adenomas.
Therefore, FCH PET-CT can be considered an important complementary modality for localization in elusive cases that are not found in the conventional modality or require reoperation due to failed surgery. In addition, because of its lower radiation dose, shorter acquisition times, and high parathyroid adenoma detection rates, FCH PET-CT can become the first-line modality for the localization of parathyroid adenomas.[20] However, further research is needed, and there are limitations since FCH PET-CT is available only in highly specialized centers.
In conclusion, we report a case of persistent unlocalizable PHPT due to retropharyngeal ectopic parathyroid adenoma, and this is the first case report of retropharyngeal ectopic parathyroid adenoma in Korea. Therefore, we suggest that the potential of retropharyngeal lesions in ectopic parathyroid adenoma should be considered in patients with unlocalizable PHPT. Additionally, FCH PET-CT could be useful as a complementary imaging modality in elusive PHPT that cannot be localized using conventional imaging techniques.
Fig. 1
Parathyroid venous sampling: parathyroid hormone level 2-fold increase at right venous drainage location. Rt., right; Lt., left; SVC, superior vena cava.
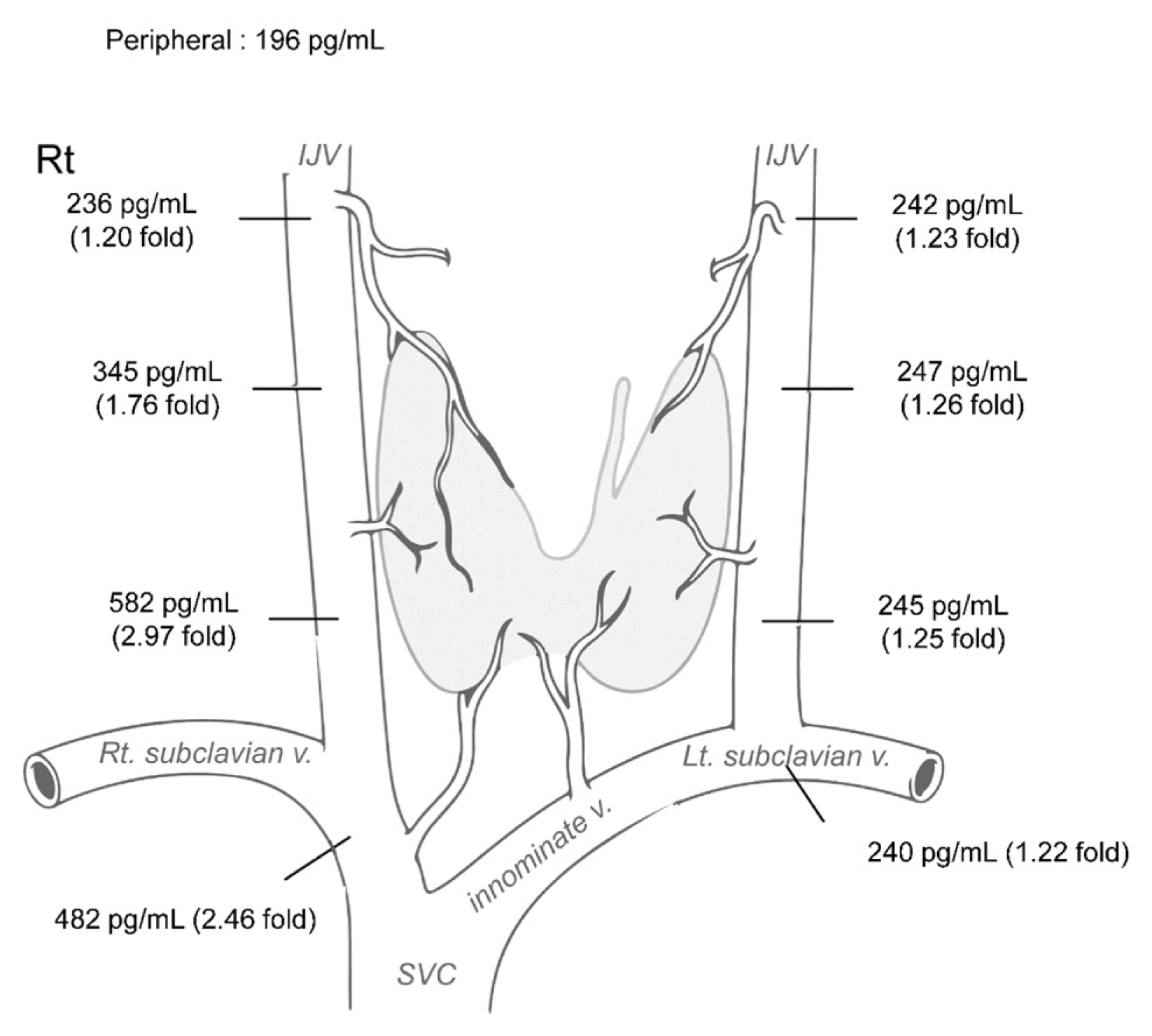
Fig. 2
Localization study results of a positive fluorocholine positron emission tomography/computed tomography, which was examined after the first surgery, show a clear focus suspect for adenoma (July 15, 2020). Sagittal view (A). Axis view (B).

REFERENCES
1. Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 2005;132:359-72. https://doi.org/10.1016/j.otohns.2004.10.005.


2. Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 2006;191:418-23. https://doi.org/10.1016/j.amjsurg.2005.10.049.


3. Wachtel H, Bartlett EK, Kelz RR, et al. Primary hyperparathyroidism with negative imaging: a significant clinical problem. Ann Surg 2014;260:474-80. discussion 80-2. https://doi.org/10.1097/sla.0000000000000875.


4. Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol 2012;33:457-68. https://doi.org/10.1016/j.amjoto.2011.10.010.



5. Iconaru L, Spinato L, Duttmann R, et al. A rare cause of persistent hyperparathyroidism. Clin Case Rep 2021;9:511-5. https://doi.org/10.1002/ccr3.3568.



6. Witteveen JE, Kievit J, van Erkel AR, et al. The role of selective venous sampling in the management of persistent hyperparathyroidism revisited. Eur J Endocrinol 2010;163:945-52. https://doi.org/10.1530/eje-10-0654.


7. Roy M, Mazeh H, Chen H, et al. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg 2013;37:102-6. https://doi.org/10.1007/s00268-012-1773-z.


8. Parikh AM, Suliburk JW, Morón FE. Imaging localization and surgical approach in the management of ectopic parathyroid adenomas. Endocr Pract 2018;24:589-98. https://doi.org/10.4158/ep-2018-0003.


9. Shin JJ, Milas M, Mitchell J, et al. Impact of localization studies and clinical scenario in patients with hyperparathyroidism being evaluated for reoperative neck surgery. Arch Surg 2011;146:1397-403. https://doi.org/10.1001/archsurg.2011.837.


10. Gallagher JW, Kelley ML, Yip L, et al. Retropharyngeal parathyroid glands: Important differences. World J Surg 2018;42:437-43. https://doi.org/10.1007/s00268-017-4236-8.


11. Broos WAM, van der Zant FM, Knol RJJ, et al. Choline PET/CT in parathyroid imaging: a systematic review. Nucl Med Commun 2019;40:96-105. https://doi.org/10.1097/mnm.0000000000000952.


12. Morland D, Lalire P, Deguelte S, et al. Added value of 18F-fluorocholine positron emission tomography-computed tomography in presurgical localization of hyperfunctioning parathyroid glands after dual tracer subtraction scintigraphy failure: A retrospective study of 47 patients. Medicine (Baltimore) 2020;99:e18681.https://doi.org/10.1097/md.0000000000018681.



13. Uslu-Beşli L, Sonmezoglu K, Teksoz S, et al. Performance of F-18 fluorocholine PET/CT for detection of hyperfunctioning parathyroid tissue in patients with elevated parathyroid hormone levels and negative or discrepant results in conventional imaging. Korean J Radiol 2020;21:236-47. https://doi.org/10.3348/kjr.2019.0268.



14. Beheshti M, Hehenwarter L, Paymani Z, et al. (18)F-Fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with (99m)Tc-MIBI or (99m)Tc-tetrofosmin SPECT/CT: a prospective dual-centre study in 100 patients. Eur J Nucl Med Mol Imaging 2018;45:1762-71. https://doi.org/10.1007/s00259-018-3980-9.



15. Thanseer N, Bhadada SK, Sood A, et al. Comparative effectiveness of ultrasonography, 99mTc-Sestamibi, and 18F-fluorocholine PET/CT in detecting parathyroid adenomas in patients with primary hyperparathyroidism. Clin Nucl Med 2017;42:e491-7. https://doi.org/10.1097/rlu.0000000000001845.


16. Maccora D, Caldarella C, Calcagni ML. (11)C-Methionine PET/CT in patients with primary hyperparathyroidism and inconclusive pre-operative imaging work-up: diagnostic accuracy and role of semi-quantitative analysis. Ann Nucl Med 2021;35:469-78. https://doi.org/10.1007/s12149-021-01584-w.


17. Noltes ME, Coester AM, van der Horst-Schrivers ANA, et al. Localization of parathyroid adenomas using (11)C-methionine pet after prior inconclusive imaging. Langenbecks Arch Surg 2017;402:1109-17. https://doi.org/10.1007/s00423-017-1549-x.

18. Traub-Weidinger T, Mayerhoefer ME, Koperek O, et al. 11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery. J Clin Endocrinol Metab 2014;99:4199-205. https://doi.org/10.1210/jc.2014-1267.


19. Bioletto F, Barale M, Parasiliti-Caprino M, et al. Comparison of the diagnostic accuracy of 18F-Fluorocholine PET and 11C-Methionine PET for parathyroid localization in primary hyperparathyroidism: a systematic review and meta-analysis. Eur J Endocrinol 2021;185:109-20. https://doi.org/10.1530/eje-21-0038.


20. Broos WAM, Wondergem M, Knol RJJ, et al. Parathyroid imaging with (18)F-fluorocholine PET/CT as a first-line imaging modality in primary hyperparathyroidism: a retrospective cohort study. EJNMMI Res 2019;9:72.https://doi.org/10.1186/s13550-019-0544-3.



- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 2,077 View
- 53 Download
- ORCID iDs
-
Hyeokjoo Jang

https://orcid.org/0000-0001-9667-2060Seunghyun Lee

https://orcid.org/0000-0001-9254-183XDahee Kim

https://orcid.org/0000-0001-7286-1334Namki Hong

https://orcid.org/0000-0002-8246-1956 - Related articles




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



