Does Bone Mineral Density Differ between Fan-Beam and Pencil-Beam?: A Meta-Analysis and Systemic Review
Article information
Abstract
Background
Dual energy X-ray absorptiometry (DXA) has evolved from pencil-beam (PB) to narrow fan-beam (FB) densitometers. We performed a meta-analysis of the available observational studies to determine how different modes of DXA affect bone mineral density (BMD) measurements.
Methods
A total of 1,233 patients (808 women) from 14 cohort studies were included. We evaluated the differences in BMD according to the DXA mode: PB and FB. Additionally, we evaluated the differences in BMD between the 2 types of FB mode: FB (Prodigy) and the most recent FB (iDXA). Pairwise meta-analysis was performed, and weighted mean differences (WMD) were calculated for (total lumbar, total hip, and total body).
Results
No significant difference was observed in total lumbar (pooled WMD, −0.013; P=0.152) and total hip BMD (pooled WMD, −0.01; P=0.889), between PB and FB. However, total body BMD was significantly lower in the PB compared to the FB group (pooled WMD, −0.014; P=0.024). No significant difference was observed in lumbar BMD (pooled WMD, −0.006; P=0.567), total hip (pooled WMD, −0.002; P=0.821), and total body (pooled WMD, 0.015; P=0.109), between Prodigy and iDXA.
Conclusions
The results of this study warrant the recommendation that correction equations should not be used when comparing BMD from different modes. Further research is still needed to highlight the ways in which differences between DXA systems can be minimized.
INTRODUCTION
Bone mineral density (BMD) is the primary determinant in the assessment of osteoporosis. Dual energy X-ray absorptiometry (DXA) is the most common modality for quantitative BMD.[1] It is a safe, accurate, and precise technique. Nevertheless, errors related to this exam are still very common and may significantly impact the final diagnosis and therapy.[2,3] Similar to other imaging modalities, DXA may be influenced by technical errors, and imaging artifacts may arise and accuracy and precision of the results may be influenced.[4]
Since its introduction in 1987, DXA has been improved over time, most evidently in reduced scan times.[5] Representatively, Pencil-beam (PB) DXA had been replaced with instruments that rely solely on fan-beam (FB) technology.[6,7] As the technology has developed, the focus of development has shifted to image quality, which has improved through advances in detector design, yielding a higher pixel density. A new detector and X-ray filter provide improved resolution and image quality by better bone edge detection.[8,9]
However, it has been verified that differences in BMD occur when PB DXA machines from the same and also from different manufacturers. Many cross-calibration studies have reported that systematic differences between the instruments may even exceed the annual biological BMD changes.[5,10–13] Considering the increased number of osteoporosis patients, it is important to determine whether and how DXA mode affect the BMD.
To the best of our knowledge, no meta-analysis has been published to determine if there are any systematic differences between 2 different modes of DXA scanner (FB and PB). Therefore, we performed a systematic review and meta-analysis of the available observational studies, evaluating the cross-calibration study difference between 2 different modes of DXA scanner, including the most recent model.
METHODS
1. Search methods for the identification of studies
This meta-analysis was conducted according to the updated guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P). Two researchers (YBH, KYD) independently searched MEDLINE (PubMed), EMBASE, and Cochrane Library databases in September 2020. An overview of the search strategy is presented in Supplementary 1. Articles that met the selection criteria (not limited to randomized studies, including prospective and case-control studies) were included in the meta-analysis. We attempted to obtain complete data for the analysis by contacting the authors of articles with insufficient or missing data.
2. Study selection criteria
Studies were screened and selected by all investigators on the basis of a priori criteria. Inclusion criteria were as follows: (1) the study was a comparative that investigated the BMD of normal adults or adolescents who underwent DXA; (2) at least one of the following main clinical outcomes was reported: the mean of BMD and standard deviation (SD). We did not include European Spine Phantom as a population.
Exclusion criteria were as follows: (1) the study accessing patients using another device: including Q-computed tomography, ultrasonography, or multi-frequency bioelectrical impedance; (2) the study reported unavailable data including intraclass correlation coefficient, coefficient of variation (CV), and standard error of measurement; (3) the study used national registry data; and (4) the article was a review, expert opinion, case report, or basic science study.
3. Outcome measures and data extraction
The primary outcome for the meta-analysis was the difference of BMD in total lumbar, total hip, and total body, which were compared between several models. The analysis was done in the 2 groups; 1. FB vs. PB 2. FB vs. most recent FB.
For every eligible study, the following data were extracted and entered into a spreadsheet by 2 reviewers: the family name of the first author, year of publication, country, number of patients, device and program, sample characteristics (age, sex ratio, body mass index), and mean and SD in BMD (g/cm2). When BMD was measured at various sites, we included data from the sites where the highest values in each site were measured because these should best reflect. PB mode includes Lunar DPX-L (GE Healthcare, Madison, WI, USA), Lunar DPX-IQ (GE Healthcare), Hologic QDR-1000, and Hologic QDR-2000. FB mode includes Hologic QDR-4500A, Lunar Prodigy (GE Healthcare). Lunar iDXA systems (GE Healthcare) is classified as the most recent model.
4. Quality assessment and publication bias
Two of the authors (YBH, KYD) independently evaluated the quality of all studies, using the Newcastle-Ottawa Scales. This tool comprises three parameters: selection, comparability, and outcome. Each parameter consists of subcategorized items; selection has a maximum of 4 stars, comparability has a maximum of 2 stars, and exposure or outcome has 3 stars. We assessed the presence of publication bias using Begg’s funnel plot and Egger’s test.
5. Statistical analysis
The primary analysis (continuous outcomes) involved a pair-wise meta-analysis of the data from all relevant studies that reported the BMD data, and the studies were weighted according to the number of included patients The effect sizes were calculated as Hedges adjusted (g) weighted mean difference (WMD), which represents the magnitude of the difference between the comparative groups, for each outcome.[10] The WMD was computed separately for all available control and treatment groups in each study. All types of effect sizes were presented along with their 95% confidence intervals (CIs).
A fixed-effects or random-effects model was used to quantify the pooled effect size of the included studies, depending on the heterogeneity of the data. Heterogeneity between comparable studies was tested using χ2 and I2 tests; P>0.1 and I2<50%, respectively, were used as established criteria to determine statistical heterogeneity. All analyses were performed using STATA software (version 14.0; Stata Corp., College Station, TX, USA). This study was exempted from Institutional Review Board review since it did not involve any human subjects.
RESULTS
1. Description of the included studies
The primary search of the databases yielded 965 records. After duplicates were removed, 560 articles were screened by title and abstract. As a result, 49 full-text articles were selected and reviewed for eligibility. A total of 14 studies were finally included in the systematic review (Fig. 1).[14–27] The studies identified for the meta-analysis involved 1,233 participants, with women comprising 808 (65.5%) of the sample population. Among the 14 studies, 8 articles compared PB and FB modes and other 6 studies compared FB and most recent FB mode (Table 1).
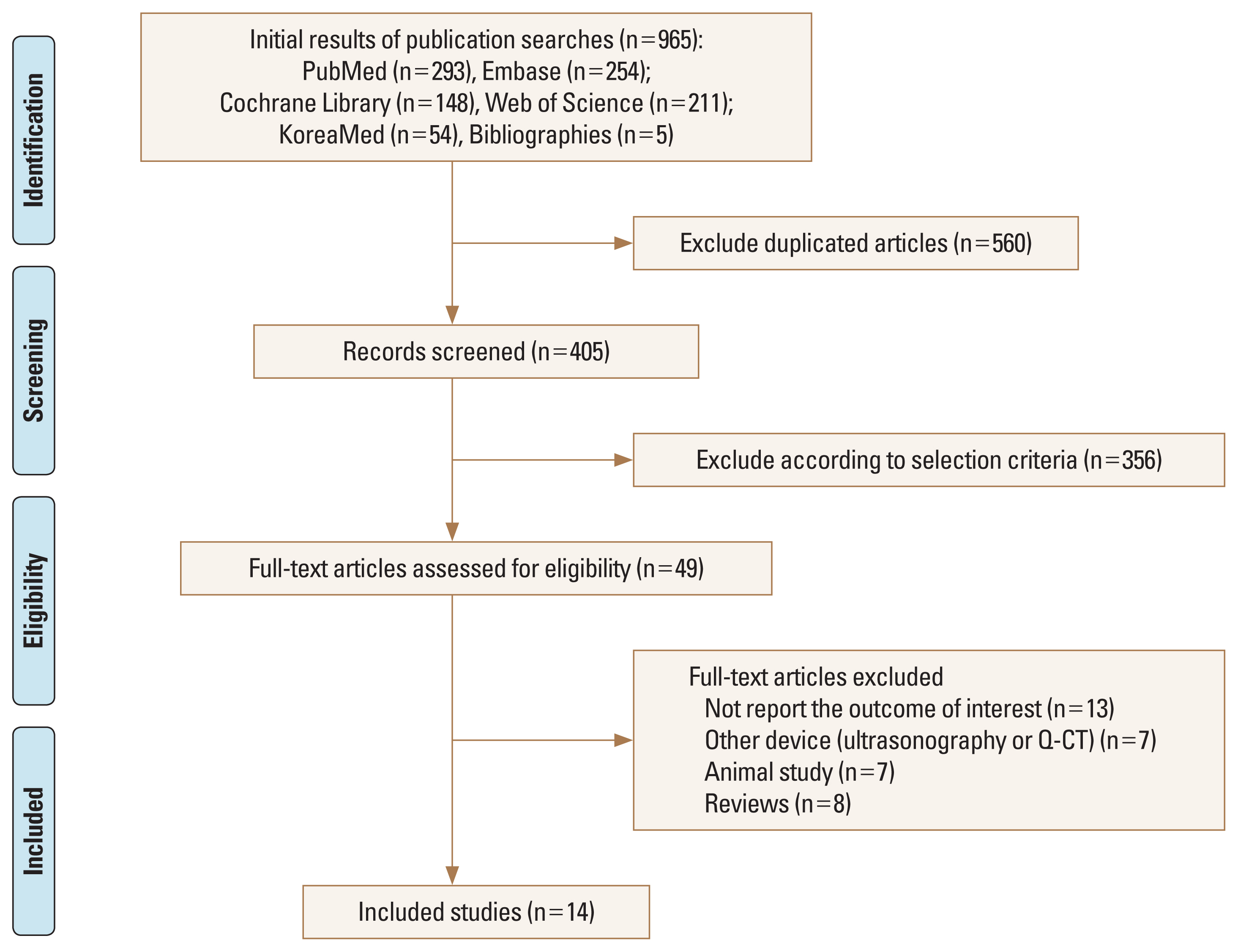
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram details the process of relevant study selection.
2. PB vs. FB
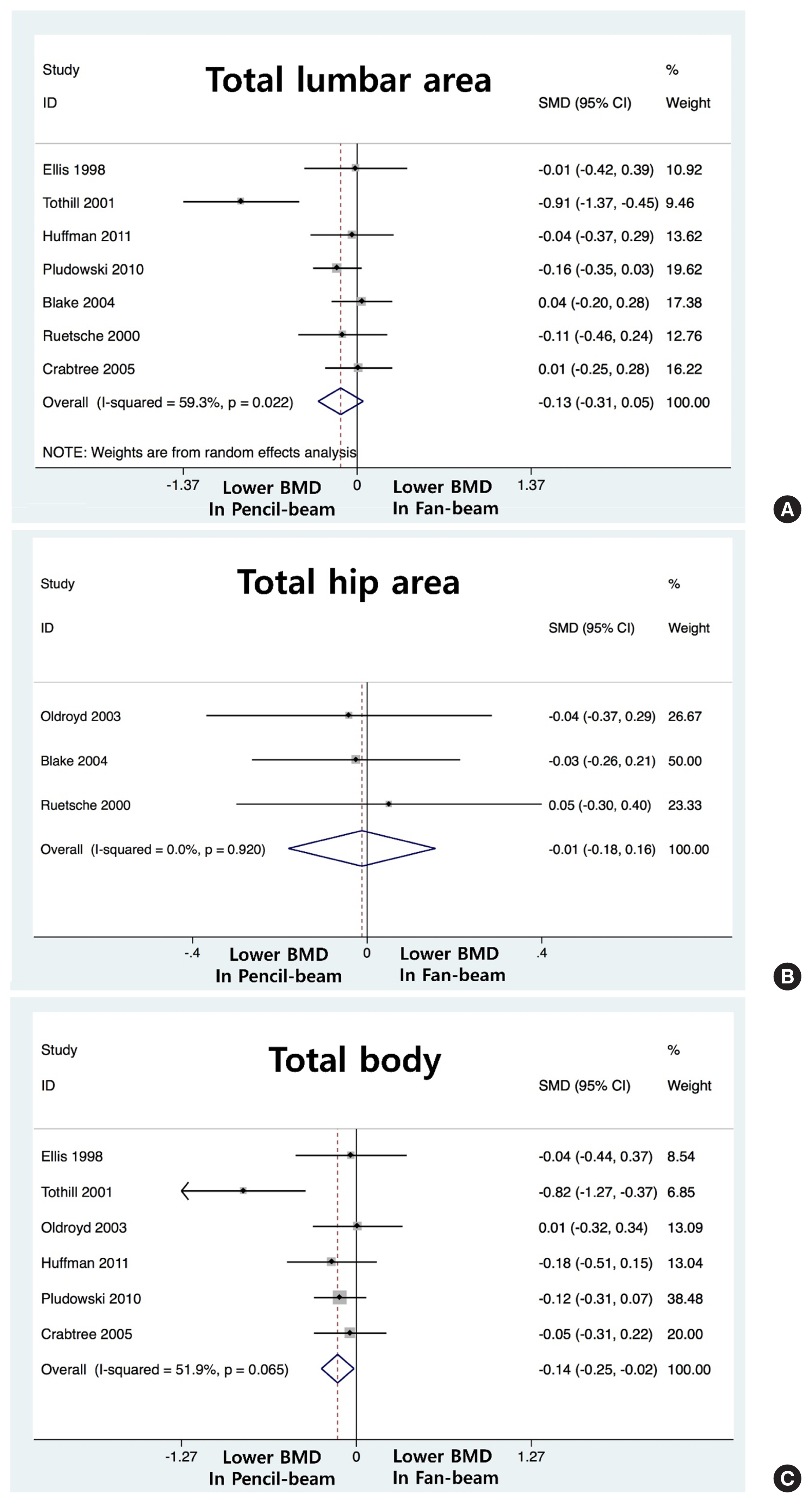
Eight studies, involving a total of 752 patients, reported data on BMD (Table 2).[18,20–26] In total lumbar BMD, there is no significant difference PB (Prodigy) and FB (pooled WMD, −0.013; 95% CI, −0.031 to 0.005; P=0.152) No significant difference also observed in total hip (pooled WMD, −0.01; 95% CI, −0.018 to 0.016; P=0.889). However, BMD was significantly lower in the PB group compared to those in the FB group in total body (pooled WMD, −0.014; 95% CI, −0.025 to −0.002; P=0.024) (Fig. 2).
3. FB vs. most recent FB
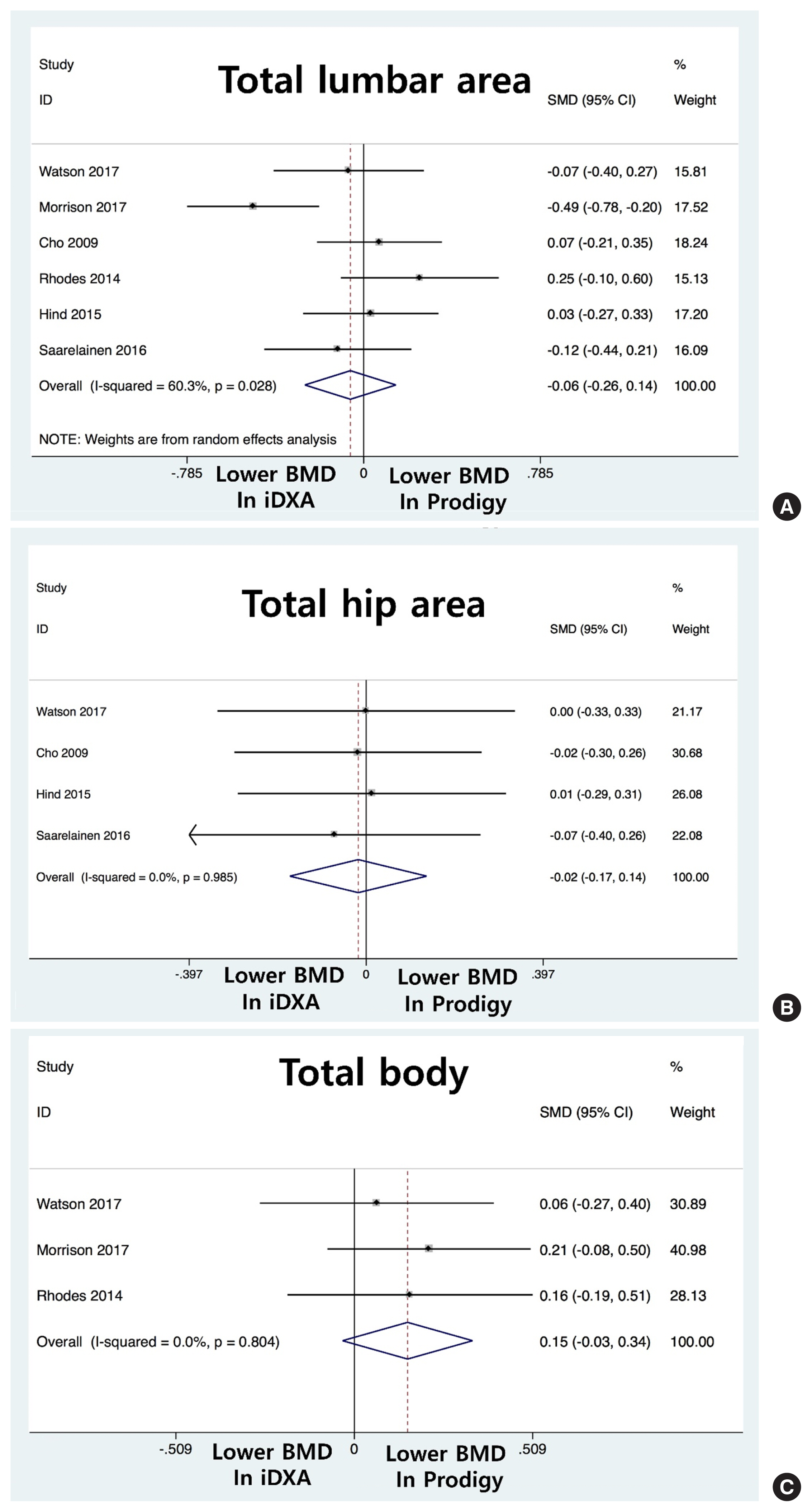
Six studies, involving a total of 481 patients, reported data on BMD.[14–17,19,27] In total lumbar BMD, there is no significant difference FB (Prodigy) and most recent FB (iDXA) (pooled WMD, −0.006; 95% CI, −0.026 to 0.014; P=0.567) No significant difference also observed in total hip (pooled WMD, −0.02; 95% CI, −0.017 to 0.14; P=0.821) and total body (pooled WMD, 0.015; 95% CI, −0.03 to 0.34; P=0.109) (Fig. 3).
4. Quality assessment and publication bias
In terms of the methodological quality, the mean value of the awarded stars was 6.5 (5 studies had 6 stars, 9 studies had 7 stars). The Begg’s funnel plot was not asymmetrical, and the P-values for bias were not significant for all outcomes (Fig. 4).
DISCUSSION
Each densitometer manufacturer uses its X-ray source and a specific methodology to obtain the 2 required energies.[22,28] Many previous studies investigating the agreement of BMD measurements between different modes of devices, but discrepancies exist among studies.[29,30] Thus, we want to investigate the continuity of the BMD calibration when a newer model replaces an older DXA scanner. In the present meta-analysis, we found no significant differences between the measured BMD regardless of the mode.
PB DXA is an established technique used for studies of bone mineral and body composition. PB technology has all but been replaced with FB systems due to faster scan times, improved image quality, and greater measurement precision.[22,31] The FB mode uses a greater photon flux and improved photon detection and consequently provides higher image resolution. Thus, FB DXA compared with PB DXA tended to overestimate BMD, whereas the area of both regions of interest was underestimated. Bone edge detection and exclusion of transverse processes through analysis probably play the key role. This discrepancy in bone edge detection represents a major explanation for BMD differences that can be found between the 2 modes.[29,32,33]
In the present study, the difference between PB and FB was only found in total BMD. It is suggested that a calibration offset was not responsible for the differences between 2 modes, as there was no significant difference in phantom scans.[7,34,35] The difference in BMD was probably owing in part to the significant difference in measured area between the 2 modes. The variation introduced by the relative position of each individual in the FB but not PB path owing to the height of the spine from the scanning table also can be more prominent in the total body area.[1,8,28, 31] And these differences between the FB and PB modes is more likely to be evident at low-density values than high-density value.[36,37]
The currently available GE Lunar system uses narrow-angle FB geometry. The excellent BMD correlation between iDXA and Prodigy is well-demonstrated in previous studies, but the inconsistencies of BMD between 2 machines are an ongoing issue.[14–16,35] The smaller pixel size further enhances the bone edge detection of iDXA, which stands out for small bones such as the hands and feet.[38] However, edge detection might be attenuated as the automated analysis techniques might place edges or regions of interest more in large bones. Further research in this field is needed for a clearer understanding of the underlying mechanism.[39]
The present study has several limitations. First, factors other than BMD, including accuracy or precision of different modes of DXA scanner have not been included in this meta-analysis. Second, we could not perform a sub-group analysis that women with osteoporosis who are known to be susceptible for erroneous to switch from one mode to another. Finally, there are numerous different brands of DXA scanners (Hologic Inc., Bedford, MA, USA) are available but our analysis was limited to 2 brands.
CONCLUSIONS
In conclusion, no significant difference of BMD was found between different modes of DXA scanner. To ensure high quality DXA acquisition and interpretation, further research is needed to highlight ways in which differences between DXA systems can be minimized.
Supplementary Information
Notes
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (NTIS Number: 9991007052).
Authors’ contributions
Conceptualization: Yoon BH, Koh YD, Yoo JI, Kim SJ, Lee GY, Park SB, Ha YC; Data curation: Yoon BH, Koh YD, Yoo JI, Kim SJ, Park SB, Ha YC; Formal analysis: Yoon BH, Koh YD, Yoo JI, Park SB, Ha YC; Investigation: Yoon BH, Koh YD, Yoo JI, Kim SJ, Lee GY, Park SB, Ha YC; Methodology: Yoon BH, Koh YD, Kim SJ, Lee GY, Park SB, Ha YC; Software: Yoon BH, Koh YD, Yoo JI, Lee GY, Park SB, Ha YC; Validation: Yoon BH, Koh YD, Lee GY, Park SB, Ha YC; Writing - original draft: Yoon BH, Koh YD, Yoo JI, Lee GY, Park SB, Ha YC; Writing - review & editing: Yoon BH, Koh YD, Yoo JI, Kim SJ, Park SB, Ha YC.
Ethics approval and consent to participate
This meta-analysis summaries previously published data and does not include new human data or tissue that require ethical approval and consent. The authors assume that the studies reviewed were conducted after ethical approval and consent, and in accordance with the Declaration of Helsinki.
Conflict of interest
Byung-Ho Yoon has been the associate editor of the Journal of Bone Metabolism since 2018. Yong-Chan Ha has been the editor-in-chief of the Journal of Bone Metabolism since 2017. No potential conflict of interest relevant to this article was reported.