Osteoporosis and Osteoporotic Fracture Fact Sheet in Korea
Article information
Abstract
Background
The socioeconomic burdens of osteoporosis and related fractures have increased in parallel with population aging. The Korea Society of Bone and Mineral Research published fact sheets on these topics in 2017, 2018, and 2019. This study provides complied epidemiological data based on these fact sheets for understanding current status of osteoporosis in Korea.
Methods
Data from the Korea National Health and Nutrition Examination Survey (2008–2011) performed by the Korea Centers for Disease Control and Prevention and from National Health Information database (2008–2016) by National Health Insurance Service of Korea was used for analyzing the prevalence and incidence of osteoporosis and related fractures, respectively, fatality rates after fractures, and prescription status of anti-osteoporotic medications (AOMs).
Results
Among Korean adults aged ≥50 years, 22.4% and 47.9% had osteopenia or osteoporosis, respectively. Incidences of osteoporotic hip, vertebral, humerus, and distal radius fractures plateaued in 2013. The cumulative incidence of subsequent fractures gradually increased over 4 years of follow-up once an osteoporotic fracture occurred. Crude fatality rates in the first 12 months after hip fracture were 14.0% for women and 21.0% for men. Only 33.5% of patients with osteoporosis took AOMs, and even after an osteoporotic fracture, only 41.9% of patients took AOMs within the following 12 months. Despite a steady increase in AOM prescriptions of ~6% per annum, only 33.2% of patients were medication compliant (medication possession ratio ≥80%) at 12 months after treatment initiation.
Conclusions
Continuous efforts are required to diagnose patients at high risk of fracture and ensure proper management in Korea.
INTRODUCTION
Osteoporosis is a metabolic bone disease characterized by reduced bone density, poor bone quality, and reduced bone strength, and thus, increases fracture risk.[1] Societal aging unavoidably increases the incidences of osteoporosis and related fractures, which are associated with enormous medical, social, and economic burdens.[2–4]
In recent Korea, the socioeconomic burdens of osteoporosis have increased and mortalities after osteoporosis-related fractures have become higher than those in the general population.[5,6] Nevertheless, the need to diagnose and actively treat osteoporosis has not received great concerns in Korea, presumably because the disease is asymptomatic before a fracture occurs. To address this issue, the Korea Society of Bone and Mineral Research (KSBMR) published osteoporosis and osteoporotic fracture fact sheets in 2017, 2018, and 2019 (available at https://www.ksbmr.org) based on the Korea National Health and Nutrition Examination Survey (KNHANES) data collated by the Korea Centers for Disease Control and Prevention (KCDC) and the National Health Information database provided by the National Health Insurance Service (NHIS) of Korea.[7–9] These fact sheets provided epidemiologic, treatment, and prescription statuses of osteoporosis and osteoporotic fractures in Korea and suggested that the increasing number of patients with osteoporosis and related fractures in Korea are closely related to the treatment status of these diseases.
Therefore, in this cross-sectional, nationwide survey study, we aimed to assemble epidemiological data about osteoporosis and osteoporotic fractures based on these fact sheets, to provide better understanding of the current situation in Korea.
METHODS
1. Study subjects
This study analyzed participants aged ≥50 years from surveys conducted during the second (2008) and third (2009) years of the fourth KNHANES and from surveys conducted during the first (2010) and second (2011) years of the fifth KNHANES for estimating the prevalence of osteopenia and osteoporosis in Korea since bone mineral density (BMD) data was available only in these periods.[10] This cross-sectional nationwide survey used a stratified, multistage, clustered probability sampling method to select a representative sample of the noninstitutionalized, civilian Korean population.[11]
This study also analyzed the National Health Information database of the Korea over the period 2008 to 2016. In Korea, 97.0% of the population is obliged to enroll in the Korea National Health Insurance Program. All clinics and hospitals submit diagnostic and medical cost data to the Health Insurance Review and Assessment Service (HIRA) so that medical costs can be refunded by the government. The remaining 3% of the population is covered by the Medical Aid Program. Thus, nearly all information about disease volumes and burdens can be obtained from the National Health Information database, with the exception of medications and procedures that are not covered by insurance.[5,12] Using this data, we calculated the incidences of osteoporotic fractures and determined treatment status of osteoporosis and related fractures and the prescription status of anti-osteoporotic medications (AOMs).
2. Definition of osteoporosis and osteoporotic fracture
Osteopenia and osteoporosis were defined in the KNHANES database using World Health Organization T-scores for Asian countries,[13] that is, 2.5 <T-score <−1.0 and T-score ≤−2.5 either in lumbar spine, femoral neck, or total hip, respectively.
In the National Health Information database, patients with osteoporosis who accessed medical services were operationally defined using 6 criteria [14]: (1) prescription of medications exclusively for osteoporosis treatment (bisphosphonate [BP], selective estrogen receptor modulators [SERMs], or calcitonin); (2) the International Classification of Diseases, Tenth Revision (ICD-10) codes for osteoporosis (M80–M82) and prescription of medications related to osteoporosis (hormones, calcium, or vitamin D); (3) elderly patients (men ≥70 years old, women ≥65 years old) with ICD-10 codes for osteoporosis; (4) a history of medications known to cause osteoporosis plus ICD-10 codes; (5) a history of disease known to cause osteoporosis plus ICD-10 codes; or a (6) osteoporosis-related fracture. Each fracture code had to be accompanied by a physician’s claim for site-specific procedure codes to enhance the specificity of the operational definitions.[15,16]
The operational definitions of osteoporotic fractures of vertebra, hip, humerus, and distal radius were made using ICD-10 codes and procedure codes using NHIS data. ICD-10 codes for vertebral fracture were; S22.0 (fracture of the thoracic spine), S22.1 (multiple fractures of the thoracic spine), S32.0 (fracture of the lumbar spine), S32.7 (multiple fractures of the lumbar spine), T080 (fracture of the spine), M48.4 (fatigue fracture of vertebra), M48.5 (collapsed vertebra), and M49.5 (collapsed vertebra). ICD codes of hip fractures were S72.0 (fracture of the femur neck) and S72.1 (trochanteric fracture). ICD-10 codes of humerus fractures were S422 (fracture of upper end of humerus), S423 (fractured shaft of humerus), and codes for distal radius fractures were S52.5 (fracture of lower end of radius) and S52.6 (fracture of lower end of both ulnar and radius).[15,16]
Subsequent osteoporotic fracture was defined as fracture of vertebra, hip, humerus, or distal radius at least 6 months after index osteoporotic fracture.[15,16]
3. Classification of AOMs
To determine prescription statuses of osteoporosis and osteoporotic fractures in Korea, we gathered information on AOM prescriptions from the NHIS data from 2011 to 2016. We analyzed SERM and BP data because they were the only medications covered by health insurance as primary therapeutic agents for osteoporosis and related fractures during this period. Daily raloxifene and bazedoxifene, which are oral medications, were included in the analysis as SERMs. Daily risedronate and alendronate and weekly risedronate, alendronate, and their cholecalciferol-combined formulations, and monthly ibandronate were included in the analysis as oral BPs. Intravenous ibandronate, which was injected 3-monthly, and intravenous zoledronic acid, which was injected annually, were also included in the analysis.
4. Statistical analyses
The primary outcomes of this study were the prevalence and incidence of osteoporosis and related fractures, respectively, fatality rates after fractures, and prescription status of AOMs. The prevalence of osteopenia and osteoporosis were calculated using a simple descriptive method using KNHANES (2008–2011) data. Numbers and incidences of osteoporotic fractures were determined using the NHIS data for the period 2008 to 2016 using a simple descriptive method. Crude fatality rates for the 12 months following hip or vertebral fractures were calculated using the NHIS data for the period 2013 to 2015. Cumulative incidences of subsequent fractures were analyzed using the NHIS data for the period 2012 to 2016. Subsequent fractures were followed up for 4 years after the index osteoporotic fracture which was occurred in 2012. AOM usage rates by patients with osteoporosis were analyzed using the NHIS data in 2010. Numbers of AOM prescriptions issued within 12 months of index osteoporotic fractures of hip, vertebra, humerus, or distal radius were obtained using the 2015 NHIS data and analyzed with respect to sex and age, fracture site, and time after fractures. AOM prescription trends were analyzed with respect to administration route and time after fracture using NHIS data for the period 2011 to 2016. The compliances to AOMs were analyzed using medication possession ratios (MPR) over 24 months using the NHIS data for the period 2012 to 2014. MPR was defined as the percentage of days an individual was in possession of prescribed medications during the whole observation period. The compliant group was defined to be composed of those with an MPR of ≥80%.
5. Ethics statement
This study protocol was approved by the Institutional Review Board of Inha University hospital. The requirement for informed consent was waived by the board because of the retrospective nature of the study and the use of de-identified data.
RESULTS
1. Epidemiologic statuses of osteoporosis and osteoporotic fracture in Korea
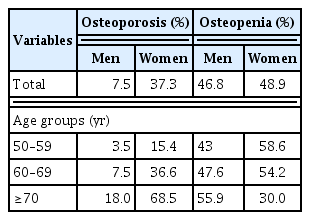
Among Korean adults aged ≥50 years, 22.4% and 47.9% had osteopenia or osteoporosis, respectively. The prevalence of osteoporosis increased with age for both genders (Table 1), and reached almost 70% in women aged ≥70 years. Furthermore, the prevalence of osteoporosis was 5 times higher in women (37.3%) than in men (7.5%), whereas the prevalence of osteopenia was similar in women (48.9%) and men (46.8%). A half of Korean men aged ≥70 years had osteopenia.
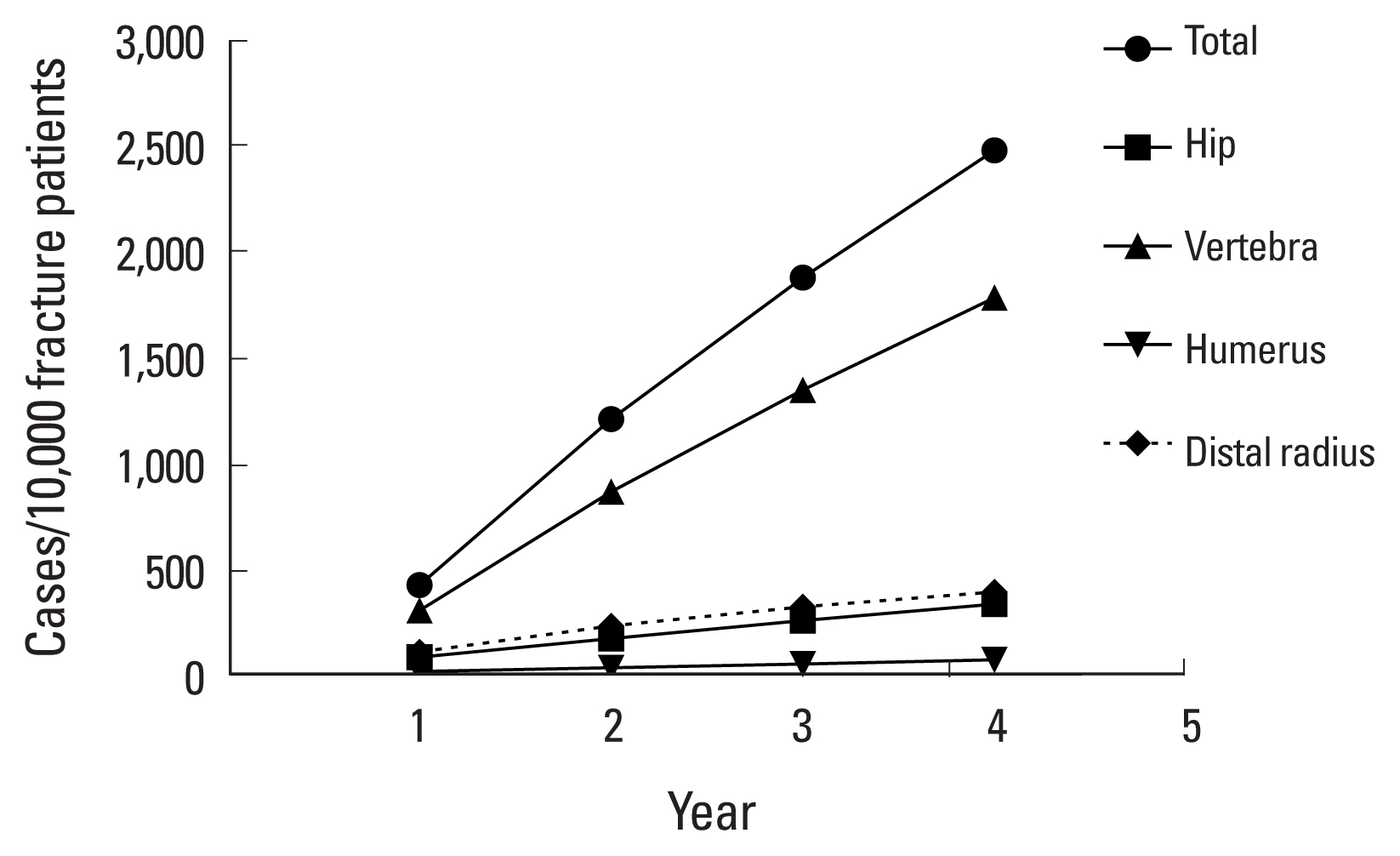
In Koreans aged ≥50 years, numbers of osteoporotic fractures at hip, vertebra, humerus, and distal radius gradually increased during 2008 to 2016 regardless of gender (Fig. 1). However, incidences of these fractures, numbers of fractures relative to the general population, did not increase after 2013. Vertebral fractures were most common in all age groups, except for women in their 50s. Distal radius fractures mainly occurred in the 50s and hip fractures rapidly increased from 70 years of age.
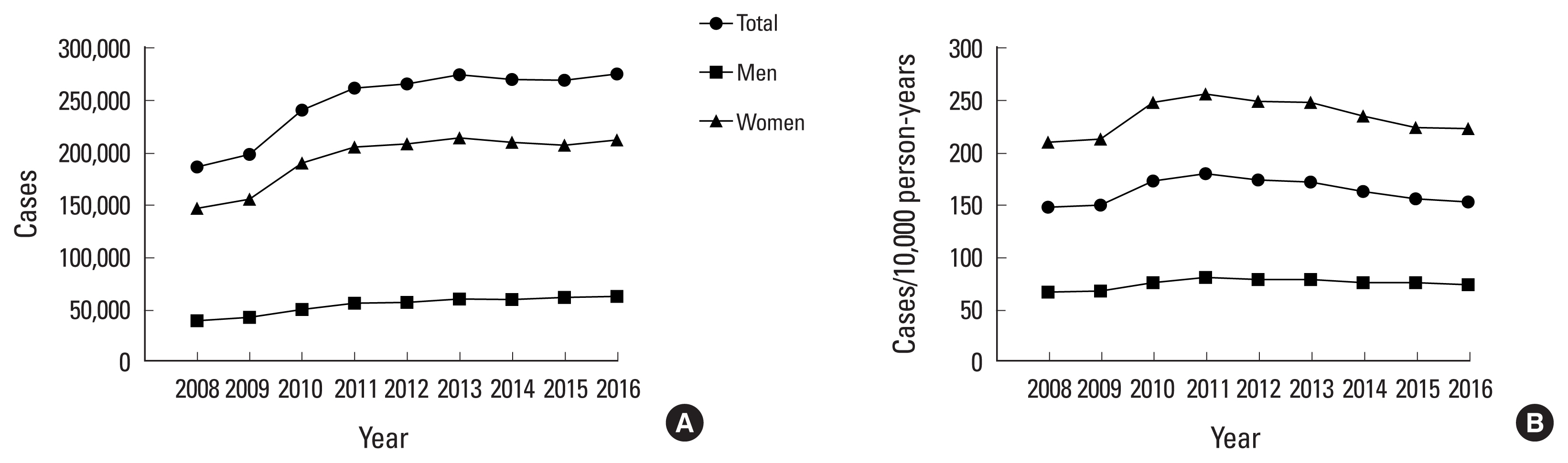
Trends in the numbers (A) and incidences (B) of osteoporotic fracture among Korean adults aged ≥50 years. Data was extracted from the National Health Insurance Service data during 2008 to 2016.
The cumulative incidence of subsequent fractures, additional fractures from 6 months after first osteoporotic fracture, gradually increased during 4 years of follow-up (Fig. 2). Subsequent fractures most frequently occurred in vertebra regardless of the sites of first osteoporotic fractures.
2. Fatalities after osteoporotic fracture in Korea
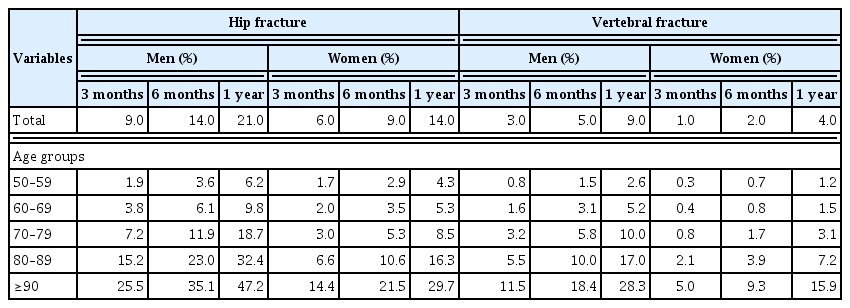
Crude fatality rates during the first 12 months after hip fracture were 14.0% for women and 21.0% for men. Fatalities after vertebral fracture occurred in 4.0% of women and 9.0% of men (Table 2). Fatality rates after hip and vertebral osteoporotic fractures were 1.5 and 2.3 times higher, respectively, in men than women. In particular, one of five elderly Korean men aged ≥70 years with a hip fracture died within a year.
3. Treatment statuses of osteoporosis and osteoporotic fracture in Korea
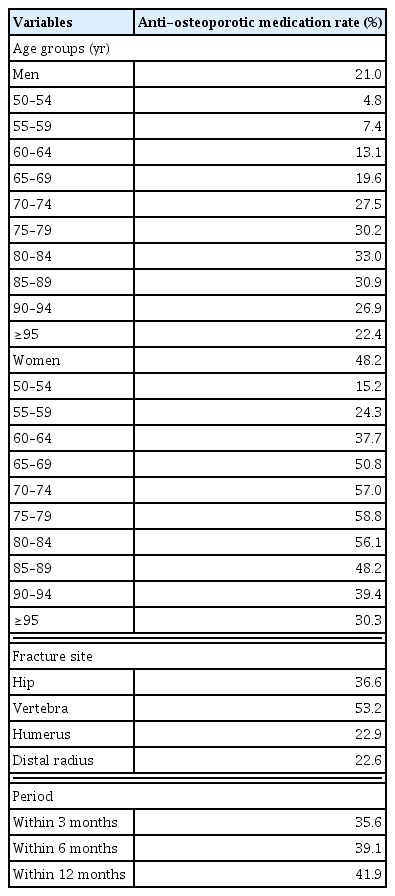
In Korea, the health service utilization rate was estimated to be ~61% among osteoporosis patients in 2010, and only 33.5% of these patients took AOMs. After osteoporotic fracture, only 41.9% of patients started taking AOMs during the first 12 months (Table 3), and the proportion of women who started taking AOMs was more than twice as high (48.2%) as that of men (21.0%). Patients aged 75 to 89 years in men and 70 to 84 years in women most commonly took medication during first 12 months after fracture. Half of the patients with a vertebral fracture took AOMs, but smaller fractions of patients with a fracture of hip, humerus, or distal radius did so. The majority of patients who took AOMs after osteoporotic fracture started their medications within 3 months of fracture.
4. Prescription statuses of AOMs in Korea
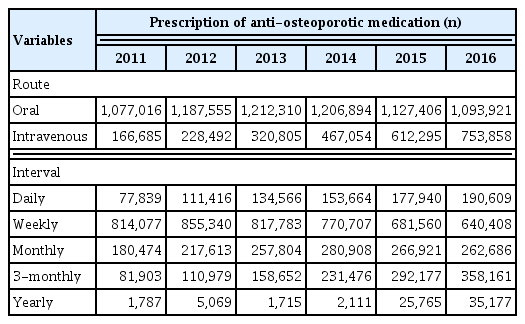
During 2011 to 2016, numbers of SERM and BP prescriptions steadily increased at an annual rate of 6%. Numbers of oral AOM prescriptions remained constant during this period, whereas those of intravenous AOMs increased to ~41% of total prescriptions in 2016 (Table 4). Regarding administration intervals, numbers of 3-monthly AOM prescriptions gradually increased, whereas number of weekly prescriptions decreased during 2011 to 2016.
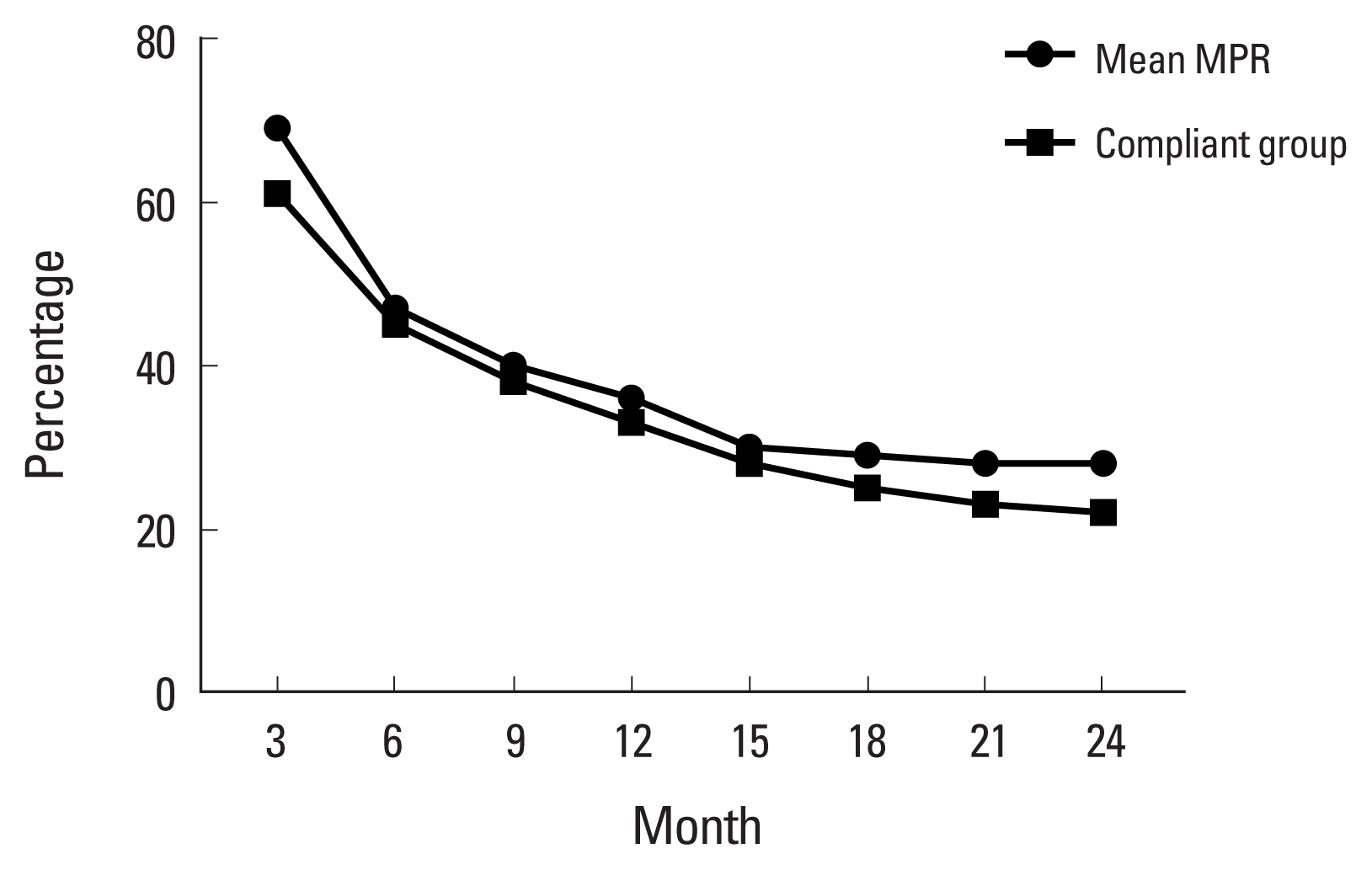
Despite the steady increase in AOM prescriptions, the MPRs of these medications were only 36.1% and 28.1% at 12 and 24 months, respectively, after treatment initiation (Fig. 3). Moreover, the percentages of patients that complied with medications after treatment initiation (MPR ≥80%) were only 33.2% and 21.5% at 12 and 24 months, respectively.
DISCUSSION
The KSBMR in cooperation with the KCDC and NHIS, has published annual fact sheets on osteoporosis and osteoporotic fractures from 2017 to provide up-to-date information on osteoporosis and osteoporotic fractures in Korea. In this present study based on these fact sheets, we found that even though the incidence rate of osteoporotic fractures finally plateaued in 2013 in Korea, there are still a lot of patients with osteoporosis or related fractures who need to be properly treated for future fracture prevention. However, the treatment and compliant rates of patients with osteoporosis or related fractures were still poor in Korea.
In Korea, about 70% of adults aged ≥50 years have been estimated to have low bone density. In fact, the prevalence of osteopenia is almost twice that of osteoporosis. Furthermore, the prevalence of osteopenia are similar in men and women, while the prevalence of osteoporosis in men is only one-fifth of that in women. It is well recognized that there are more fractures in patients with BMD T-scores between −2.5 and −1.0 (osteopenia) than those with BMD T-scores of ≤−2.5 (osteoporosis) because there are so many more patients in this category.[17] Therefore, it is a well-accepted management concept that strategies for preventing fractures should be initiated from the diagnosis of osteopenia.[18] Moreover, patients with osteopenia with clinical risk factors of fractures are now regarded to be as deserving of treatment as patients with osteoporosis.[4, 19,20] However, no recommendation has been issued regarding the treatment of patients with osteopenia in Korea and AOMs such as SERMs and BPs are not currently covered by health insurance in this patient population.
Between 2008 and 2016 in Korea, although the absolute number of osteoporotic fractures increased year-on-year from 186,488 to 275,131, fracture incidence (numbers of osteoporotic fractures per 10,000 of the general population) has remained constant from 2013. Thus, the observed increase in the number of osteoporotic fractures during this period is probably due to societal aging.[21] In this regard, continuous efforts have been made to provide medical treatment to osteoporosis patients in Korea. In particular, in 2011, health insurance coverage for AOMs in osteoporosis patients was expanded from a BMD T-score of ≤−3.0 to ≤−2.5. Accordingly, changes in Korean health care policy for patients with osteoporosis have enabled more active treatment of those at high risk of fracture.[14]
A previous osteoporotic fracture history is the strongest risk factor of future fracture.[22–27] Approximately half of individuals that have experienced one osteoporotic fracture are known to experience another, and the number of fractures experienced exponentially increases the risk of future fracture. Although few studies have addressed the incidence of subsequent fracture, a recent study found that the overall cumulative incidence of subsequent fracture following an index fracture was 12% at 24 months.[28] Similarly, this present study has reported cumulative incidences for subsequent fracture of 12.1% and 24.8% during 24 and 48 months of follow-up in Korea, respectively, regardless of index fracture type, although vertebrae were most frequently affected by secondary fractures. Since subsequent fractures impose enormous socioeconomic burdens and have relatively high mortality rates,[29–31] it is important that patients with an osteoporotic fracture history be identified and provided proper management to prevent future fractures.
Nevertheless, only a relatively small number of patients are being treated for osteoporosis in Korea. In particular, only 4 of 10 patients with an osteoporotic fracture history take AOMs during the 12 months after fracture. The percentage of vertebral fracture patients prescribed AOMs during the 12 months after fracture was higher (53.2%) than for those with a hip (36.6%), humerus (22.9%), or distal radius (22.6%) fracture. The under-treatment of patients at high risk for osteoporotic fracture, including those with a fracture history, is a worldwide management problem.[32–34] This treatment gap results from the under-diagnosis of osteoporosis, concerns about the adverse effects of medications (e.g., medication-related osteonecrosis of the jaw [MRONJ] and atypical femoral fracture [AFF]), misunderstanding of the benefit to risk ratio of medication, and poor coordination between health care systems. In particular, by missing the opportunity to respond properly to first fractures, healthcare systems worldwide have failed to prevent second and subsequent fractures.[35]
In this regard, several efforts have been made in Korea to improve the management of patients with osteoporosis and related fractures. Specifically, Korea participates in “World Osteoporosis Day”, an annual campaign dedicated to raising global awareness of the need to prevent, diagnose, and treat osteoporosis and related bone diseases (iofbonehealth.org/world-osteoporosis-day-2017). Moreover, the KSBMR published a position statement regarding the adverse effects of AOMs, including MRONJ and AFF, in 2015 [36] that contained precise definitions and the epidemiologies of these adverse effects and suggested treatment and preventative strategies. Recently, the KSBMR also established a “Fracture Liaison Service (FLS)”, a coordinator-based, secondary fracture prevention service implemented by health care systems. This service is designed to close the care gap for fracture patients (80% of whom are currently not offered screening or treatment for osteoporosis) and to enhance communication between health care providers by providing a care pathway for the treatment of fragility fracture patients.[37] The FLS committee of the KSBMR recently published a guidebook on this coordinator-based secondary fracture prevention [38] and is also running a pilot project aimed at developing regular coordinator training program.
BPs remain the mainstay medical treatment of osteoporosis for a long time, despite the relatively recent introductions of new anti-resorptives and anabolic agents. BPs that are administered via new routes or at extended intervals have also been developed that offer advantages over conventional treatments. BPs administered intravenously alleviate gastrointestinal discomfort in many elderly patients exposed to polypharmacy, and BPs administered weekly, monthly, 3-monthly, or annually reduce the burden of taking medications. In this regard, numbers of prescriptions for intravenous or less frequently administered AOMs have steadily increased in Korea. Nevertheless, compliance with AOMs is still poor as fewer than a half of patients prescribed AOMs comply with medication requirements during the first 12 months. This low compliance in Korea, which is also a worldwide problem, may stem from insufficient recognition of the importance of osteoporosis management in terms of maintaining quality of life and reducing the enormous socioeconomic burdens associated with this disease. Moreover, exaggerated concerns regarding the rare complications of BPs may lead to the passive treatment of osteoporosis.[35]
This is the first epidemiologic study to be conducted on osteoporosis and related fractures in Korea using nationally representative data from KNHANES and NHIS. This study accurately presents the current epidemiologic status and statuses of treatment and prescriptions in patients with osteoporosis and related fractures in Korea, as we were able to investigate the whole Korean population using health insurance and health aid service data. However, this study also had its limitations. There are disadvantages of insurance claim database such as incorrect diagnostic coding, misclassification error by patient defining algorithms, and failure to include prescription outside insurance coverage. Specifically regarding medication analysis, we could not retrieve data regarding AOMs taken by osteopenia patients. Moreover, since insurance policy was just expanded to cover denosumab as a first-line treatment for osteoporosis in 2019 and teriparatide is still approved as a second-line treatment, we were unable to analyze the prescription patterns of these newly developed AOMs.
As the population in Korea ages, it appears inevitable that the number of patients with osteopenia, osteoporosis, and related fractures will continue to increase. Fortunately, the incidence rate of osteoporotic fractures among Korean has plateaued, but treatment and compliance rates are still poor among osteoporotic fracture patients. Therefore, continuous efforts are required to identify patients at high risk of osteoporotic fracture and to ensure these patients be provided proper management that reinforces the need to comply with treatment.
Acknowledgments
This work was supported by Korean Society for Bone and Mineral Research. National Health Information Database (NHIS-2020-1-525) was provided by the National Health Insurance Service (NHIS) of Korea. The authors would like to thank the NHIS for cooperation.
Notes
Ethics approval and consent to participate
The study protocol conformed to the ethical guidelines of the World Medical Association Declaration of Helsinki and was approved by the Institutional Review Board of Inha University hospital.
Conflict of interest
This study used National Health Information Database (NHIS-2020-1-525) made by National Health Insurance Service (NHIS). The authors declare no conflict of interest with NHIS.