Intravenous Zoledronate for a Patient with Paget's Disease
Article information
Abstract
Paget's disease (PD) of bone is characterized by increase of bone resorption by atypical osteoclasts, followed by rapid new bone formation resulting in a disorganized mosaic bone. Although the pathophysiology is not fully understood, bisphosphonate, which is a potent anti-resorptive agent for treatment of osteoporosis, have been the most effective agents available for the treatment of PD. We report a case of PD of bone in a 49-year-old woman patient, who was treated with intravenous zoledronate.
INTRODUCTION
Paget's disease (PD) of bone is a focal, progressive disorder of accelerated bone remodeling and can lead to bone pain and several complications, including deformities, fractures, and secondary osteoarthritis.[1,2,3,4] Although the pathophysiology of PD is very complicated and not well known, the primary lesion is the abnormally increased and activated osteoclast in PD.[1,2,3,4]
Bisphosphonates, which is the most potent anti-resorptive drug, have been the most effective agents available for the treatment of PD.[1] Among the bisphosphonates for osteoporosis treatment, zoledronate is a nitrogen-bound intravenous bisphosphonate with highest potency and longest administration interval.[5,6,7] There has been no study on zoledronate for PD of bone in Korea.
We reported a patient with PD, who had inadequate responses to therapy with pamidronate, has had a clinical remission with intravenous zoledronate.
CASE
In May, 2010, a 49-year-old woman presented with 4 year history of both buttock pain. The onset of the pain had been insidious with no significant history of trauma. The pain was localized to both buttock and lower back. She was referred to our hospital for further evaluation from other clinics. Laboratory findings revealed that serum alkaline phosphatase (ALP) level was 57 IU/L (reference range, 30 to 115 IU/L). A bone scan, which undergone at outside hospital 4 year ago, confirmed pagetic changes in the left ilium (Fig. 1). And, pelvis anterior-posterior radiograph obtained at our hospital revealed a typical mosaic pattern of PD in her pubic and left ilium (Fig. 2).
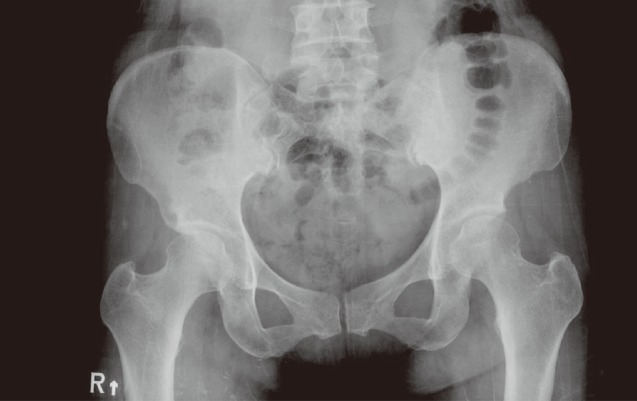
Pelvis anterior-posterior radiograph revealed a mosaic pattern in left pubis and ilium around sacroiliac joint.
She had no family history of PD. Physical examination revealed the tenderness at the left iliac crest and posterior iliosacral joint. Her weight was 61.4 kg, height was 162 cm, and body mass index was 23.4 kg/m2. Range of motion at left hip was decreased due to pain, and she walked with a mild limp.
Although the level of ALP was within reference range, pamidronate treatment was started orally for 3 months, because she had a severe pain. However, her pain intensity level increased. The ALP was 44 IU/L, and bone scan show still hot uptake in her both ilium and lumbar vertebrae (Fig. 3).

The bone scan, which was obtained 3 months after administration of oral pamidronate, showed increased uptake in left ilium and acetabulum.
Subsequently, she received intravenous zoledronate (5 mg) in a single dose at August, 2010. After this treatment, we evaluated clinical and biochemical remission and improvement in bone scan. Three months after administration zoledronate, ALP decreased 26 IU/L, and a severe pain and limping gait disappeared. Six months after intravenous zoledronate, ALP decreased 21 U/L, and bone scan showed the improvement, which means a response of zoledronate (Fig. 4). After then, she was lost to follow-up.

The bone scan, which was obtained 6 months after administration of intravenous zoledronate, had no increased uptake in pelvis.
In March, 2012, she visited our hospital again, because of left hip pain. Although ALP was 34 IU/L, and bone scan showed hot uptake in both ilium and lumbar vertebrae (Fig. 5).

Bone scan showed hot uptake in both ilium and lumbar vertebrae, when she visited again our hospital 19 months after administration of intravenous zoledronate.
One year after second zoledronate, ALP was 37 IU/L, and the bone scan also improved (Fig. 6). She had no pain, and refused the third injection of zoledronate. There was no adverse drug reaction during the treatments.
DISCUSSION
We report a patient with PD of bone, resistant to pamidronate treatment in whom intravenous zoledronate produced clinical remission and an improvement in the bone scan during 3 years.
In United States population over 55 years, the incidence of PD is estimated to approximately 2-5%.[1,4,8] However, the incidence is very low, and had not been well-known in Korea.
The biochemical marker for early diagnosis and monitoring is serum ALP. Serum ALP is an indicator of osteoblast activity and the primary marker for assessment of PD.[2,3] However, this patient had low ALP at initial presentation, which cannot allow physician to suspect PD by a screening laboratory profile. Bone scan can be used as a complementary method to diagnose and monitor the activity of PD.
Recent treatment guidelines recommend an use of bisphosphonate for PD to prevent disease progression and associated-complications, even in asymptomatic patients, especially with critical anatomic location such as skull, spine, weight-bearing bones, or the acetabular regions.[1]
Oral bisphosphonate has been traditionally used for this, but compliance of oral bisphosphonate is too low, because of complex ingesting methods and gastro-esophageal irritation.[9,10,11] Therefore, annually intravenous zoledronate could be alternative optional. In addition, zoledronate is a bisphosphonate with highest potency.[9]
A clinical trial reported that a single 5 mg zoledronic acid infusion normalized ALP levels in 89% of patients, compared with 58% in the control group administered oral risedronate, 30 mg/day for 60 for 2 months.[12] The therapeutic response was maintained for the longer period in zoledronate group.[13]
Although advantages of zoledronate include the convenience of a 15 minute infusion, approximately 40% of patients experienced zoledronate-associated symptoms (flu-like illness, pyrexia, myalgia, arthralgia, bone pain), typically within the first 3 days after the infusion, with most symptoms resolving within 3 days after onset.[14,15]
This case study demonstrated that a patient with PD who had been treated unsuccessfully with oral bisphosphonates was effectively treated with a 5 mg infusion of zoledronate. The ability of zoledronate to provide a sustained remission offers many advantages for patients with PD and may lead to considerable benefits for the long term in preventing or minimizing complications.
Notes
No potential conflict of interest relevant to this article was reported.

