A Case of Teriparatide on Pregnancy-Induced Osteoporosis
Article information
Abstract
Pregnancy-induced osteoporosis is a rare disorder characterized by fragility fracture and low bone mineral density (BMD) during or shortly after pregnancy, and its etiology is still unclear. We experienced a case of a 39-year-old woman who suffered from lumbago 3 months after delivery. Biochemical evidence of increased bone resorption is observed without secondary causes of osteoporosis. Radiologic examination showed multiple compression fractures on her lumbar vertebrae. We report a case of patient with pregnancy-induced osteoporosis improved her clinical symptom, BMD and bone turnover marker after teriparatide therapy.
INTRODUCTION
Osteoporosis is common in people aged 50 and over, but the disease can strike the younger age groups. Osteoporotic fracture associated with pregnancy and breast feeding is rare, so its treatment is not well understood, not to mention the natural course of treated osteoporotic fracture.[1] Pregnancy-induced osteoporosis was reported in 1955 for the first time.[2] Parathyroid hormone-related protein (PTHrP) is likely to be responsible for osteoporotic fracture.[3] The symptom is also claimed as the consequence of disturbed bone formation during pregnancy in which bone resorption continued until mid-pregnancy while bone formation remains slow until 28 weeks.[4] We experienced a case of a woman who had osteoporotic fracture three months after delivery without a history of significant disease. Teriparatide was used for treatment.
CASE
Patient: A 39-year-old woman
Chief complaint: Low back pain
Current medical history: A woman began to have low back pain at 2 months after vaginal birth. She had no significant past medical history. Her low back pain exacerbated at 3 months after delivery. Magnetic resonance imaging (MRI), provided by the previous hospital, revealed multiple compression fractures (L1-L5) on her lumbar vertebrae. On admission, the patient was breastfeeding after her first birth.
Family history: Her father had lung cancer.
Past history: The patient had sympathectomy due to hyperhidrosis. However, she had no history of other drug.
Physical findings: On physical examination, her blood pressure was 110/70 mmHg and her pulse was 72/minute. Height was 156 cm, weight was 50 kg, and body mass index was 20.5 kg/m2. No lump felt in thyroid gland. Neither abdominal tenderness nor hepatosplenomegaly was detected. Tenderness was present on lower back.
Laboratory findings: Peripheral blood examination revealed white blood cells 7,660/µL, hemoglobin 13.4 g/dL, platelet 218,000/µL, aspartate aminotransferase (AST)/alanine aminotransferase (ALT) 19/24 IU/L, blood urea nitrogen (BUN) 18.0 mg/dL, creatinine 0.76 mg/dL, calcium 9.7 mg/dL (8.2-10.4) , and phosphorus 4.2 mg/dL (1.9-4.4). Thyroid stimulating hormone (TSH) was 1.73 µIU/mL (0.35-5.58) and free thyroxine was 1.49 ng/dL (0.89-1.76). Luteinizing hormone was 0.8 mIU/mL (0.1-6.0), estrogen was 51.23 pg/mL (150-350), estradiol was 34.85 pg/mL (22-250), 24-hour urine cortisol was 26.51 µg/day (10-121), and urinary calcium was 259 mg/day (100-300). Parathyroid hormone (PTH) was 10.6 pg/mL (14-72), serum 25-hydroxy-vitamin D was 28.80 ng/mL (30-100), serum alkaline phosphatase was 332 IU/L (104-280), osteocalcin was 30.46 ng/mL (11-30), and cross-linked C-terminal telopeptide of type I collagen (CTX) was 1.15 ng/mL (0.01-0.60).
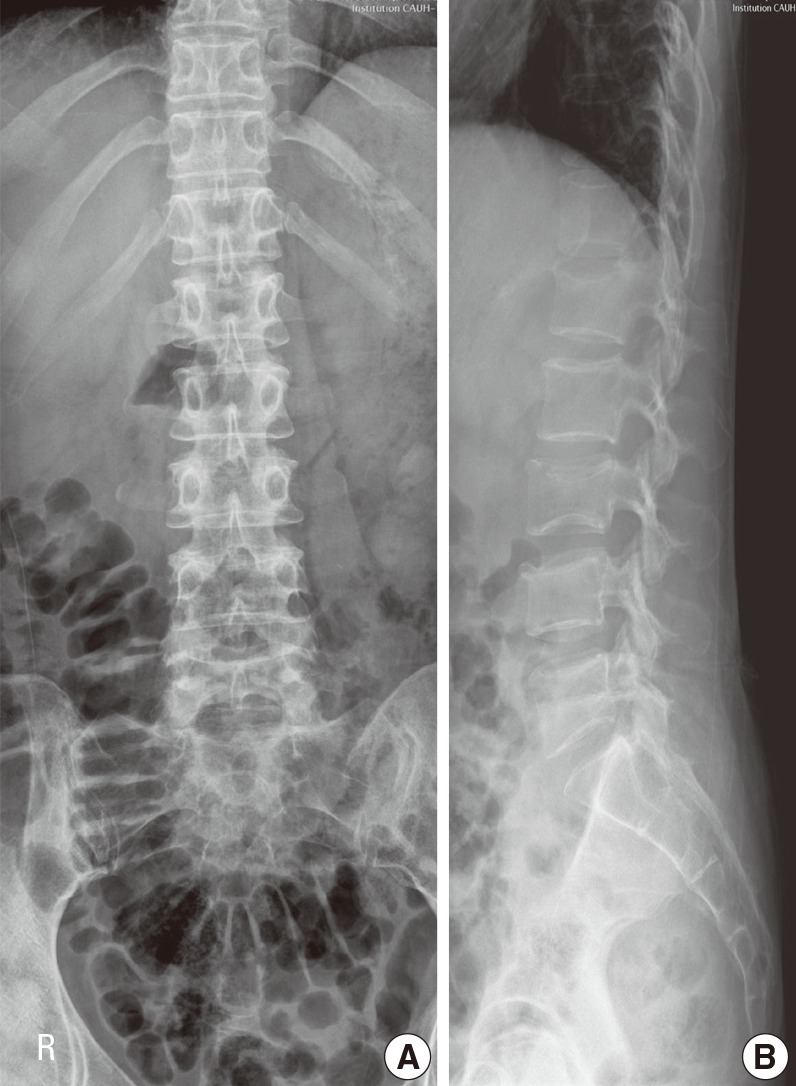
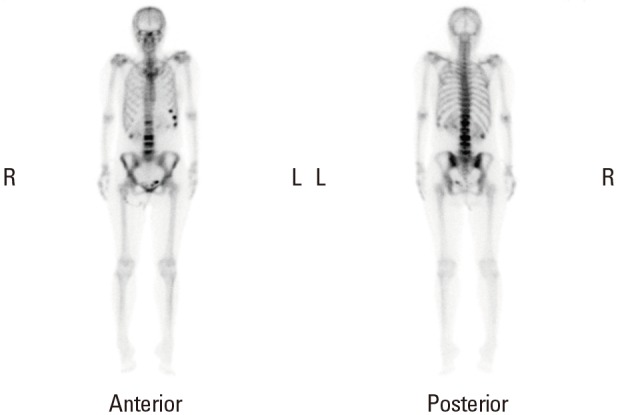
Radiologic examination: Lateral view of lumbar vertebrae detected a loss of vertebral height in L1-L5 (Fig. 1). MRI exhibited multiple compression fractures in the same lumbar region (Fig. 2). Bone scan revealed increased uptake in left 6-8th ribs and L1-L5 (Fig. 3). On dual energy X-ray absorptiometry (DXA), L1-L4 Z-score was -2.2, and BMD value was 0.855 g/cm2. However, it was difficult to assess the condition correctly due to compression fractures. Femur neck Z-score was -1.4 on both sides, and BMD value was 0.754 g/cm2 (Table 1).
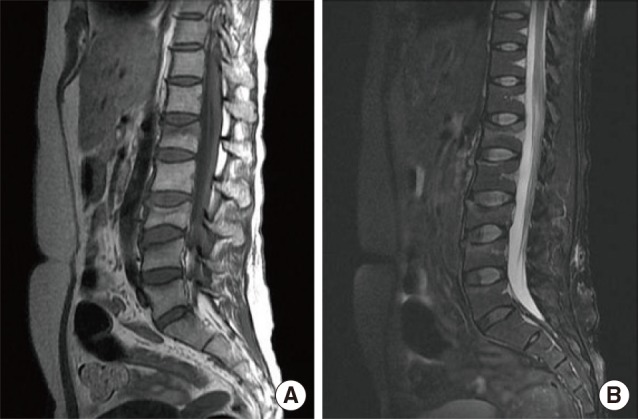
Magnetic resonance imaging (T1 and T2 weighted images) of lumbar spine. (A) T1 weighted images show ill-defined hypointense lesion in L1-L5. (B) T2 weighted images show high signal intensity in the lesion.

Changes of bone mineral density by dual energy X-ray absorptiometry and biochemical parameters after teriparatide therapy
Treatment and outcome: After the diagnosis of pregnancy-associated multiple compression fractures, the patient was given oral bromocriptine 2.5 mg once daily for a week to stop breast feeding. Once breastfeeding stopped, the patient was given oral administration of calcium 3,000 mg and vitamin D (cholecalciferol 800 IU) and daily subcutaneous injection of 20 µg of teriparatide. In 4-month follow-up, serum calcium was 9.4 mg/dL, phosphorus was 3.5 mg/dL and, PTH was 19.1 pg/mL, showing normal ranges. Serum osteocalcin increased to 62.24 ng/mL, compared with the baseline value, whereas alkaline phosphatase decreased to 239 IU/L, CTX 0.608 ng/mL. The Z-score and mean BMD values improved to -0.7 and 1.040 g/cm2, respectively. Low back pain gone and teriparatide has been prescribed for 10 months at outpatient clinic during follow-up examination.
DISCUSSION
Patients with pregnancy-induced osteoporosis may develop secondary osteoporosis. Therefore, it is necessary to identify a patient's past history, including any previous surgeries and drug treatment and conduct endocrine evaluations, including hyperthyroidism, hyperparathyroidism and Cushing's syndrome. Among 35 patients with pregnancy-induced osteoporosis, 6 patients developed secondary osteoporosis.[5]
Although the association between pregnancy and bone metabolism is uncertain, calcium is required by unborn babies to build their bone during the third trimester of pregnancy. An average daily amount around 200-250 mg of calcium is transferred to the fetus even during breast-feeding period.[6] Calcium and vitamin D deficiency arises as the number of pregnancies and total breastfeeding time increase.[7] Pregnancy-induced osteoporosis is caused by mechanisms in addition to amount of calcium intake and postpartum amenorrhea period. It is estimated that 33% of patients who have compression fractures as a result of pregnancy-associated osteoporosis may develop secondary fractures.[8]
Treatment options for pregnancy-associated osteoporosis include medications, calcium and vitamin D supplementation and stop of breast-feeding. When calcium and vitamin D supplementation was combined with stop of breastfeeding, lumbar BMD increased by 6% in 8 months and 9.5% in 2-4 years.[8] As alendronate was additionally administered, lumbar BMD increased to 5-15%.[9] It also increased to 23% in 2 years in another study.[1] The use of teriparatides instead of bisphosphonates for 18 months increased lumbar BMD to 36%.[10] Bisphosphonates inhibit the resorption of bone. While its half-life is short, its affinity for bone is high, extending the half-life to several years. This means that bisphosphonate passes through the placenta during the half-year period.[11] Thus bisphosphonate can affect fertile women despite its efficacy in osteoporosis. Pamidronate, a class of bisphosphonates, resulted in a transient hypocalcemia of the fetus when it was administered to a woman before her pregnancy.[12]
On the contrary, teriparatide proved to be effective in increasing BMD but reducing the risk of fractures in men and postmenopausal women. Teriparatide is classified as category C in the pregnancy category system used by the U. S. Food and Drug Administration (FDA).[13] The half-life of teriparatide is an hour, which is much shorter than that of bisphosphonates, making it safe for fertile women. Teriparatide 20 µg was administered once a day to women with pregnancy-associated osteoporosis for 18 months.[10,14] For postpartum patients with lumbago, osteoporotic fracture should be suspected. Teriparatide can be a therapeutic option for the treatment of pregnancy-associated osteoporosis.
Notes
No potential conflict of interest relevant to this article was reported.